Background
Surface electromyography (sEMG) is a technique which is used to analyze and record electrical activity of the skeletal muscles during the voluntary or involuntary movement. It records the myoelectric signal by surface electrode which is placed on the skin on the target muscle. These signals reflect collective electrical activity of the multiple motor units. This signal gives the important information about the muscle function, coordination, fatigue and neuromuscular diseases.
Electromyography (EMG) was developed in early 20th century initially by using needle electrodes for localized recordings. sEMG is less invasive and more suitable technique for the superficial muscle assessment compared to the intramuscular EMG (iEMG). Some factors like skin impendence and electrode placement may affect the quality of the signal. The application of sEMG in neuromuscular diseases is used to evaluate muscle activation patterns and for biofeedback training.
Muscle contractions produce electrical impulses that are detected by sEMG electrodes on the skin’s surface. The quality of sEMG recordings is determined by electrode location, skin preparation, crosstalk and signal processing procedures. Proper alignment with muscle fibers, skin preparation and precise signal filtering are needed for optimum signal detection. Rectification, filtering and normalizing are methods for extracting relevant data from raw sEMG signals.
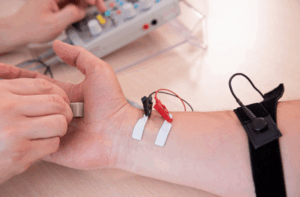
sEMG technique with electrode placed on the skin
Indications
Neuromuscular disorders: sEMG is used to assess the muscle activation abnormality in diseases like muscular dystrophy, amyotrophic lateral sclerosis (ALS), myasthenia gravis, and peripheral neuropathies. It helps to evaluate the muscle weakness, coordinate deficits and disease progression.
Movement disorders: Patients who have diseases like Parkinson’s, dystonia, and spasticity-related disease can experience the abnormal muscle activation pattern. sEMG can help to identify the involuntary muscle contraction, tremors and rigidity of the treatment choices.
Post-Stroke Motor Recovery: Patient who is recovering from the stroke may experience the impaired motor control and spasticity. sEMG is used in the rehabilitation to assess the muscle activity, guide therapy and give biofeedback for the motor re-education.
Chronic Pain and Myofascial diseases: sEMG is used to evaluate the muscle tension and dysfunction in patients who have chronic pain diseases like fibromyalgia, lower back pain, and temporomandibular joint dysfunction (TMJD). It helps to diagnose the myofascial trigger points and guide in biofeedback therapy.
Gait and Postural Analysis: Patients who have abnormal gait patterns because of musculoskeletal or neurological disease can benefit from the sEMG analysis. It helps to identify the muscle imbalance and improper activation pattern to improve the rehabilitation results.
Contraindications
Open Wounds or Skin Infections: sEMG must not be performed on areas with open wounds, burns or active skin infections because by placing the electrodes on compromised skin can lead to irritation, infection or inaccurate signal acquisition.
Severe Edema or Swelling: Patients with significant swelling in the affected area may experience changes in tissue conductivity, which can lead to poor signal quality and unreliable muscle activity results.
Implanted Electrical Devices: Patients who have pacemakers, implantable cardioverter-defibrillators (ICDs) or deep brain stimulators can be at risk of electrical interference.
Severe Neurological Disorders with Uncontrolled Muscle Activity: In diseases like severe spasticity, involuntary muscle contractions or persistent tremors like advanced Parkinson’s disease or dystonia, excessive muscle movements can change the accuracy of the results of sEMG.
Allergy to Electrode Adhesives or Gels: Patients who have known allergic reactions to electrode adhesives or conductive gels may develop skin irritation, redness or dermatitis which needs the use of alternative hypoallergenic materials.
Thick Scar Tissue Over Target Muscles: Scar tissue from earlier surgeries or injuries may affect the electrode adherence and alter signal transmission which can lead to inaccurate sEMG results.
Severe Cognitive or Behavioral Disorders: Patients who have severe cognitive impairment, anxiety or movement disorders which can prevent cooperation during testing may not tolerate the procedure and can lead to unreliable results.
Outcomes
Equipment
Surface electrodes: Pre-gelled disposable electrodes, dry electrodes and reusable silver or silver chloride (Ag/AgCl) electrodes
Electrode placement accessories: Skin preparation materials like alcohol wipes, abrasive gel or skin prep pads, electrode adhesive or tapes
sEMG amplifier: Differential amplifiers, wireless amplifiers
Signal processing and acquisition system: Analog-to-digital converter (ADC), high or low-pass filters, sampling rate controller
Data acquisition software: Real-time visualization software, analysis software, machine learning integration
Portable sEMG systems: wireless sEMG sensors, EMG-integrated wearable devices
Patient preparation
Obtain a complete history of any existing medical conditions, such as neuromuscular, skin, and implanted diseases. Explain the technique to the patient and address any concerns and ensure cooperation.
Assess for any contraindications like open wounds, acute edema or electrode adhesive allergies.
Clean the skin with alcohol wipes, abrasive gel or fine sandpaper.
Remove extra hair for better electrode adherence and signal quality.
Patient position
Make sure the patient is lying or seated in a relaxed posture based on the muscles which is being assess.
Give instruction to the patient to minimize the unnecessary movements to prevent the signal artifacts.
If assessment involve the dynamic movements, make sure patient understands the necessity of the motions for the accurate results.
Technique
Step 1: Patient preparation
The patient is prepared for a sEMG by explaining the procedure, addressing any concerns and checking their medical history and contraindications.
Clean the skin, shave excess hair and lightly apply an abrasive gel or pad.
The patient is advised to minimize unnecessary movements and understand the required motions for accurate data collection.
Step 2: Electrode placement
Place the electrodes on the target muscle and make sure a standard inter-electrode distance and use a reference electrode on a bony or electrically neutral area.
Secure the electrodes with the adhesive patches or medical tape and if using reusable electrodes, apply conductive gel before the placement to prevent movement during procedure.
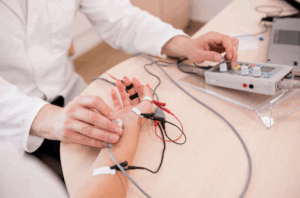
Placement of the electrode on target muscle
Step 3: Signal Acquisition and Calibration
Connect the electrode which can lead to the amplifier by using shielded cables. Check baseline signals on the software display for noise and minimal artifacts. Calibrate the system by adjusting gain, filter settings and sampling rate. Perform a test contraction to verify muscle activity response.
Step 4: Conduct the procedure
Instruct the patient on movements and record the EMG signals and monitor for artifacts. Consistent effort is needed and multiple trials are necessary for reliable data collection. Artifacts may include movement artifacts, electrode displacement or electrical interference.
Step 5: Analyze the data
Process the sEMG signals and apply filters to remove noise, normalize data, extract key parameters, measure the muscle activation levels, time of contractions and fatigue patterns. Compare the results with baseline values and interpret the results to know the clinical or research objectives.
Step 6: Post-procedure care
Remove electrodes, clean skin and check for irritation. Store equipment properly. Discard the disposable electrodes and clean reusable ones. Provide post-test instructions, inform patients of follow-up assessments and discuss improvements and future training sessions for biofeedback.
Complications
Skin irritation and allergic reactions: Some patients may experience skin irritation due to electrode adhesives, conductive gels, or prolonged electrode placement like redness, itching, rash or mild discomfort.
Artifacts: Signal interference because of improper electrode placement, excessive movement or electrical noise from nearby devices like Unstable or unclear EMG signals, excessive baseline noise or artifacts in recording.
Motion artifacts: Sudden or excessive movements which can lead to electrode displacement or mechanical noise.
Electrode displacement: Poor adhesion due to sweat, movement or improper skin preparation,
Muscle fatigue and discomfort: Repetitive muscle contractions during prolonged sEMG testing can lead to symptoms like muscle soreness, fatigue or temporary discomfort.
Psychological factors like anxiety or stress-induced artifacts: Patients may feel anxious or tense leading to involuntary muscle contractions and altered sEMG results.

Surface electromyography (sEMG) is a technique which is used to analyze and record electrical activity of the skeletal muscles during the voluntary or involuntary movement. It records the myoelectric signal by surface electrode which is placed on the skin on the target muscle. These signals reflect collective electrical activity of the multiple motor units. This signal gives the important information about the muscle function, coordination, fatigue and neuromuscular diseases.
Electromyography (EMG) was developed in early 20th century initially by using needle electrodes for localized recordings. sEMG is less invasive and more suitable technique for the superficial muscle assessment compared to the intramuscular EMG (iEMG). Some factors like skin impendence and electrode placement may affect the quality of the signal. The application of sEMG in neuromuscular diseases is used to evaluate muscle activation patterns and for biofeedback training.
Muscle contractions produce electrical impulses that are detected by sEMG electrodes on the skin’s surface. The quality of sEMG recordings is determined by electrode location, skin preparation, crosstalk and signal processing procedures. Proper alignment with muscle fibers, skin preparation and precise signal filtering are needed for optimum signal detection. Rectification, filtering and normalizing are methods for extracting relevant data from raw sEMG signals.
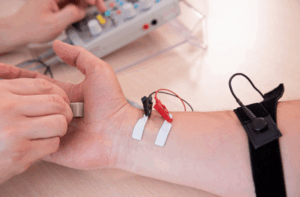
sEMG technique with electrode placed on the skin
Neuromuscular disorders: sEMG is used to assess the muscle activation abnormality in diseases like muscular dystrophy, amyotrophic lateral sclerosis (ALS), myasthenia gravis, and peripheral neuropathies. It helps to evaluate the muscle weakness, coordinate deficits and disease progression.
Movement disorders: Patients who have diseases like Parkinson’s, dystonia, and spasticity-related disease can experience the abnormal muscle activation pattern. sEMG can help to identify the involuntary muscle contraction, tremors and rigidity of the treatment choices.
Post-Stroke Motor Recovery: Patient who is recovering from the stroke may experience the impaired motor control and spasticity. sEMG is used in the rehabilitation to assess the muscle activity, guide therapy and give biofeedback for the motor re-education.
Chronic Pain and Myofascial diseases: sEMG is used to evaluate the muscle tension and dysfunction in patients who have chronic pain diseases like fibromyalgia, lower back pain, and temporomandibular joint dysfunction (TMJD). It helps to diagnose the myofascial trigger points and guide in biofeedback therapy.
Gait and Postural Analysis: Patients who have abnormal gait patterns because of musculoskeletal or neurological disease can benefit from the sEMG analysis. It helps to identify the muscle imbalance and improper activation pattern to improve the rehabilitation results.
Open Wounds or Skin Infections: sEMG must not be performed on areas with open wounds, burns or active skin infections because by placing the electrodes on compromised skin can lead to irritation, infection or inaccurate signal acquisition.
Severe Edema or Swelling: Patients with significant swelling in the affected area may experience changes in tissue conductivity, which can lead to poor signal quality and unreliable muscle activity results.
Implanted Electrical Devices: Patients who have pacemakers, implantable cardioverter-defibrillators (ICDs) or deep brain stimulators can be at risk of electrical interference.
Severe Neurological Disorders with Uncontrolled Muscle Activity: In diseases like severe spasticity, involuntary muscle contractions or persistent tremors like advanced Parkinson’s disease or dystonia, excessive muscle movements can change the accuracy of the results of sEMG.
Allergy to Electrode Adhesives or Gels: Patients who have known allergic reactions to electrode adhesives or conductive gels may develop skin irritation, redness or dermatitis which needs the use of alternative hypoallergenic materials.
Thick Scar Tissue Over Target Muscles: Scar tissue from earlier surgeries or injuries may affect the electrode adherence and alter signal transmission which can lead to inaccurate sEMG results.
Severe Cognitive or Behavioral Disorders: Patients who have severe cognitive impairment, anxiety or movement disorders which can prevent cooperation during testing may not tolerate the procedure and can lead to unreliable results.
Surface electrodes: Pre-gelled disposable electrodes, dry electrodes and reusable silver or silver chloride (Ag/AgCl) electrodes
Electrode placement accessories: Skin preparation materials like alcohol wipes, abrasive gel or skin prep pads, electrode adhesive or tapes
sEMG amplifier: Differential amplifiers, wireless amplifiers
Signal processing and acquisition system: Analog-to-digital converter (ADC), high or low-pass filters, sampling rate controller
Data acquisition software: Real-time visualization software, analysis software, machine learning integration
Portable sEMG systems: wireless sEMG sensors, EMG-integrated wearable devices
Obtain a complete history of any existing medical conditions, such as neuromuscular, skin, and implanted diseases. Explain the technique to the patient and address any concerns and ensure cooperation.
Assess for any contraindications like open wounds, acute edema or electrode adhesive allergies.
Clean the skin with alcohol wipes, abrasive gel or fine sandpaper.
Remove extra hair for better electrode adherence and signal quality.
Make sure the patient is lying or seated in a relaxed posture based on the muscles which is being assess.
Give instruction to the patient to minimize the unnecessary movements to prevent the signal artifacts.
If assessment involve the dynamic movements, make sure patient understands the necessity of the motions for the accurate results.
Step 1: Patient preparation
The patient is prepared for a sEMG by explaining the procedure, addressing any concerns and checking their medical history and contraindications.
Clean the skin, shave excess hair and lightly apply an abrasive gel or pad.
The patient is advised to minimize unnecessary movements and understand the required motions for accurate data collection.
Step 2: Electrode placement
Place the electrodes on the target muscle and make sure a standard inter-electrode distance and use a reference electrode on a bony or electrically neutral area.
Secure the electrodes with the adhesive patches or medical tape and if using reusable electrodes, apply conductive gel before the placement to prevent movement during procedure.
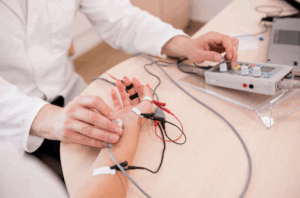
Placement of the electrode on target muscle
Step 3: Signal Acquisition and Calibration
Connect the electrode which can lead to the amplifier by using shielded cables. Check baseline signals on the software display for noise and minimal artifacts. Calibrate the system by adjusting gain, filter settings and sampling rate. Perform a test contraction to verify muscle activity response.
Step 4: Conduct the procedure
Instruct the patient on movements and record the EMG signals and monitor for artifacts. Consistent effort is needed and multiple trials are necessary for reliable data collection. Artifacts may include movement artifacts, electrode displacement or electrical interference.
Step 5: Analyze the data
Process the sEMG signals and apply filters to remove noise, normalize data, extract key parameters, measure the muscle activation levels, time of contractions and fatigue patterns. Compare the results with baseline values and interpret the results to know the clinical or research objectives.
Step 6: Post-procedure care
Remove electrodes, clean skin and check for irritation. Store equipment properly. Discard the disposable electrodes and clean reusable ones. Provide post-test instructions, inform patients of follow-up assessments and discuss improvements and future training sessions for biofeedback.
Skin irritation and allergic reactions: Some patients may experience skin irritation due to electrode adhesives, conductive gels, or prolonged electrode placement like redness, itching, rash or mild discomfort.
Artifacts: Signal interference because of improper electrode placement, excessive movement or electrical noise from nearby devices like Unstable or unclear EMG signals, excessive baseline noise or artifacts in recording.
Motion artifacts: Sudden or excessive movements which can lead to electrode displacement or mechanical noise.
Electrode displacement: Poor adhesion due to sweat, movement or improper skin preparation,
Muscle fatigue and discomfort: Repetitive muscle contractions during prolonged sEMG testing can lead to symptoms like muscle soreness, fatigue or temporary discomfort.
Psychological factors like anxiety or stress-induced artifacts: Patients may feel anxious or tense leading to involuntary muscle contractions and altered sEMG results.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



