Background
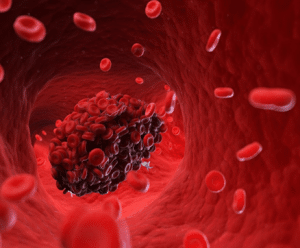
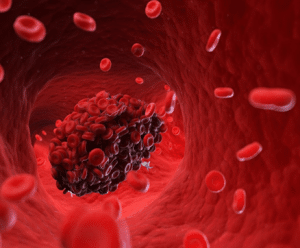
Thrombectomy is a procedure carried out on patients whereby a thrombus or blood clot is taken out of the blood vessel. This procedure is important, especially where the blood clots develop within the arteries hence affecting blood circulation and causing conditions like a stroke or pulmonary embolism.
There are several techniques by which thrombectomy may be done; the way this procedure will be conducted will depend on the location and nature of the clot, conduction of the patient, and the expertise of the personnel.
Indications
Acute Ischemic Stroke:
Large vessel occlusion (LVO) in the anterior circulation (e.g., middle cerebral artery).
Delivered in a short time frame of up to 24 hours from the onset of symptoms based on clinical and imaging features.
Deep Vein Thrombosis (DVT):
PT with proximal DVT mainly when the limb viability is at risk for compromise.
It applies to such complications as Phlegmasia cerulea dolens, which can be regarded as a severe form of DVT that is characterized by massive edema and pain.
Pulmonary Embolism (PE):
This immense PE leads to rapid heart rate and falls in blood pressure.
Volume overload of sub pulmonary area with sign of RV strain or failure.
Peripheral Arterial Thrombosis:
Acute limb ischemia with viable or threatened limb.
Formation of a blood clot within the lumen of one of the large arteries with a substantial decrease in blood flow.
Renal Vein Thrombosis:
Severe cases associated with reduced kidney function or manifestations that are considered significant.
Contraindications
Severe comorbid conditions:
The following categories of patients is at a higher risk as far as the procedure is concerned: Extensive disease involving the neck or upper chest, general poor health status, advanced cancer in the head and neck region, liver failure, renal failure or other severe systematic diseases.
Patient preparation:
Large infarct size: Severe cerebral edema, as evidenced by imaging, may exclude the potential of thrombectomy.
Severe neurological deficits: However, if the patient has very severe deficits or a very poor prognosis of functional recovery, thrombectomy could be contraindicated.
Unfavorable vascular anatomy: Possible reasons include anatomic features that make it difficult or impossible to get to the clot which usually are contraindications to the procedure.
Outcomes
Equipment
Stent Retrievers
Aspiration Catheters
Balloon Catheters
Penumbra System
Thrombectomy Devices
Angiojet
Stent retrieval tool
Patient preparation
Neurological Evaluation: Assess the patient clinically for neurological deficits that could define the severity of the stroke using NIH Stroke Scale (NIHSS).
Imaging: Perform computerised tomography, magnetic resonance imaging or computer assisted tomography angiography to determine the clot presence and the amount of brain tissue loss.
Discussion: Should inform the patient and the family members about the procedure, risks, benefits and the other feasible approaches.
Consent Form: Written informed consent is necessary from the patient.
Medical History and Physical Examination
History: Discuss the patient’s past health history with previous stroke experiences, other illnesses, and medication intake.
Physical Exam: Preliminary examinations; Specialized physical examination; Imaging studies and other tests.
Patient position
The preferred position is supine.
Mechanical thrombectomy
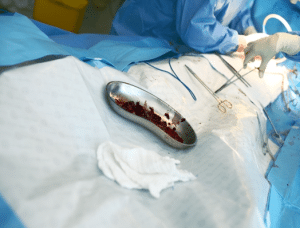
Removal of blood clots from vessel during surgery
Step 1: Preparation:
Imaging and Diagnosis: A contrast CT scan of the head is also critical to confirm if the person has had a stroke, locate the clot’s position, and evaluate if the patient qualifies for a mechanical thrombectomy procedure or not.
Step 2: Anesthesia: General anesthesia as well as loco-regional anesthesia combined with sedation based on the state of the patient.
Step 3: Access: The interventional radiologist finds a vein of entry normally in the groin. To gain access to the femoral artery a small puncture is made through administering local anesthesia.
Step 4: Catheter Insertion and Clot Removal:
Catheter Navigation: A very thin and soft tube is inserted through the identified point and then navigated towards the arteries and towards the clot in the brain.
Thrombectomy technique Selection: When it comes to clot removal, different devices are utilized most used device is:
Stent Retriever: After a little metallic net is deployed, the clot gets trapped in it. To remove the clot, it is expanded and contracted.
Aspiration Catheter: A thin, hollow tube with suction capacity is employed to directly aspirate the clot out of the patient’s body.
Combination Therapy: Often, it is possible it uses both techniques of clearing the blockage, when it is very complicated one.
Clot Removal and Blood Flow Restoration: Once the clot is trapped or sucked off, the devices are removed, and the blood flow in the artery is again restored.
Step 5: Angiogram Confirmation: The last angiogram is done to check for recoiling and removal of the clot and ensure the blood flow is back to normal.
Step 6: Closure and Monitoring:
Catheter Removal: The guiding catheter after being threaded right into the femoral artery is withdrawn as carefully as it was introduced.
Closure of Access Site: The wound site can be closed either with a closure device or by applying pressure to help control bleeding.
Post-Procedural Care: The patient is admitted to an intensive care unit where they are observed for possible adverse effects and healing process. Anticoagulant medicines to stop future clots may be given.
Laboratory tests:
Complete Blood Count (CBC):
Diagnose a condition of the person’s health and evaluates diseases like anemia and any type of infection in the body.
Coagulation Profile:
Prothrombin Time (PT): A test that helps in determining the amount of time that a blood takes to clot or thicken.
Activated Partial Thromboplastin Time (aPTT): Describes and grades the intrinsic pathway of coagulation.
International Normalized Ratio (INR): Becomes especially more valuable when adjusting PT results to normal and is principally implemented for patients under anticoagulant drugs such as warfarin.
Complications
Intracranial Hemorrhage: The symptom of this condition is bleeding in the brain.
Perforation: A structural imperfection of the blood vessel which may be life-threatening as it leads to blood loss to the patient.
Embolization:
Distal Embolization: It’s possible for the clot, or parts of it, to separate and travel to other parts of the circulatory system, obstructing further blood flow.
Non-target Embolization: To other parts of the body apart from those required in the process.
Infection: There is likelihood to develop an infection at the spot of the catheter’s positioning or from the interior of the vascular system.
Reperfusion Injury:
The damage of the tissue occurring from the re-opening of blood vessels when the oxygen supply gets restored to that particular tissue after some time it was tied off.
Allergic Reactions:
Side effects interacting with the contrast dyes or any other medication that the patient may have taken during the process.
Bleeding:
Access Site Hematoma: Haemorrhaging or developing of bruises commonly at the area where the catheter was placed.

Thrombectomy is a procedure carried out on patients whereby a thrombus or blood clot is taken out of the blood vessel. This procedure is important, especially where the blood clots develop within the arteries hence affecting blood circulation and causing conditions like a stroke or pulmonary embolism.
There are several techniques by which thrombectomy may be done; the way this procedure will be conducted will depend on the location and nature of the clot, conduction of the patient, and the expertise of the personnel.
Acute Ischemic Stroke:
Large vessel occlusion (LVO) in the anterior circulation (e.g., middle cerebral artery).
Delivered in a short time frame of up to 24 hours from the onset of symptoms based on clinical and imaging features.
Deep Vein Thrombosis (DVT):
PT with proximal DVT mainly when the limb viability is at risk for compromise.
It applies to such complications as Phlegmasia cerulea dolens, which can be regarded as a severe form of DVT that is characterized by massive edema and pain.
Pulmonary Embolism (PE):
This immense PE leads to rapid heart rate and falls in blood pressure.
Volume overload of sub pulmonary area with sign of RV strain or failure.
Peripheral Arterial Thrombosis:
Acute limb ischemia with viable or threatened limb.
Formation of a blood clot within the lumen of one of the large arteries with a substantial decrease in blood flow.
Renal Vein Thrombosis:
Severe cases associated with reduced kidney function or manifestations that are considered significant.
Severe comorbid conditions:
The following categories of patients is at a higher risk as far as the procedure is concerned: Extensive disease involving the neck or upper chest, general poor health status, advanced cancer in the head and neck region, liver failure, renal failure or other severe systematic diseases.
Patient preparation:
Large infarct size: Severe cerebral edema, as evidenced by imaging, may exclude the potential of thrombectomy.
Severe neurological deficits: However, if the patient has very severe deficits or a very poor prognosis of functional recovery, thrombectomy could be contraindicated.
Unfavorable vascular anatomy: Possible reasons include anatomic features that make it difficult or impossible to get to the clot which usually are contraindications to the procedure.
Stent Retrievers
Aspiration Catheters
Balloon Catheters
Penumbra System
Thrombectomy Devices
Angiojet
Stent retrieval tool
Neurological Evaluation: Assess the patient clinically for neurological deficits that could define the severity of the stroke using NIH Stroke Scale (NIHSS).
Imaging: Perform computerised tomography, magnetic resonance imaging or computer assisted tomography angiography to determine the clot presence and the amount of brain tissue loss.
Discussion: Should inform the patient and the family members about the procedure, risks, benefits and the other feasible approaches.
Consent Form: Written informed consent is necessary from the patient.
History: Discuss the patient’s past health history with previous stroke experiences, other illnesses, and medication intake.
Physical Exam: Preliminary examinations; Specialized physical examination; Imaging studies and other tests.
Patient position
The preferred position is supine.
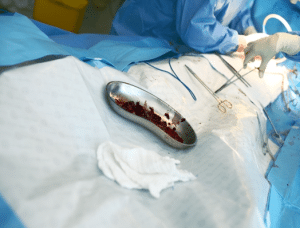
Removal of blood clots from vessel during surgery
Step 1: Preparation:
Imaging and Diagnosis: A contrast CT scan of the head is also critical to confirm if the person has had a stroke, locate the clot’s position, and evaluate if the patient qualifies for a mechanical thrombectomy procedure or not.
Step 2: Anesthesia: General anesthesia as well as loco-regional anesthesia combined with sedation based on the state of the patient.
Step 3: Access: The interventional radiologist finds a vein of entry normally in the groin. To gain access to the femoral artery a small puncture is made through administering local anesthesia.
Step 4: Catheter Insertion and Clot Removal:
Catheter Navigation: A very thin and soft tube is inserted through the identified point and then navigated towards the arteries and towards the clot in the brain.
Thrombectomy technique Selection: When it comes to clot removal, different devices are utilized most used device is:
Stent Retriever: After a little metallic net is deployed, the clot gets trapped in it. To remove the clot, it is expanded and contracted.
Aspiration Catheter: A thin, hollow tube with suction capacity is employed to directly aspirate the clot out of the patient’s body.
Combination Therapy: Often, it is possible it uses both techniques of clearing the blockage, when it is very complicated one.
Clot Removal and Blood Flow Restoration: Once the clot is trapped or sucked off, the devices are removed, and the blood flow in the artery is again restored.
Step 5: Angiogram Confirmation: The last angiogram is done to check for recoiling and removal of the clot and ensure the blood flow is back to normal.
Step 6: Closure and Monitoring:
Catheter Removal: The guiding catheter after being threaded right into the femoral artery is withdrawn as carefully as it was introduced.
Closure of Access Site: The wound site can be closed either with a closure device or by applying pressure to help control bleeding.
Post-Procedural Care: The patient is admitted to an intensive care unit where they are observed for possible adverse effects and healing process. Anticoagulant medicines to stop future clots may be given.
Laboratory tests:
Complete Blood Count (CBC):
Diagnose a condition of the person’s health and evaluates diseases like anemia and any type of infection in the body.
Coagulation Profile:
Prothrombin Time (PT): A test that helps in determining the amount of time that a blood takes to clot or thicken.
Activated Partial Thromboplastin Time (aPTT): Describes and grades the intrinsic pathway of coagulation.
International Normalized Ratio (INR): Becomes especially more valuable when adjusting PT results to normal and is principally implemented for patients under anticoagulant drugs such as warfarin.
Intracranial Hemorrhage: The symptom of this condition is bleeding in the brain.
Perforation: A structural imperfection of the blood vessel which may be life-threatening as it leads to blood loss to the patient.
Embolization:
Distal Embolization: It’s possible for the clot, or parts of it, to separate and travel to other parts of the circulatory system, obstructing further blood flow.
Non-target Embolization: To other parts of the body apart from those required in the process.
Infection: There is likelihood to develop an infection at the spot of the catheter’s positioning or from the interior of the vascular system.
Reperfusion Injury:
The damage of the tissue occurring from the re-opening of blood vessels when the oxygen supply gets restored to that particular tissue after some time it was tied off.
Allergic Reactions:
Side effects interacting with the contrast dyes or any other medication that the patient may have taken during the process.
Bleeding:
Access Site Hematoma: Haemorrhaging or developing of bruises commonly at the area where the catheter was placed.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



