Background
The thyroid gland has been known historically; the Romans described it as the gland with the shape of a shield. The first known reference to thyroid masses dates to the 12th and 13th centuries. From the twelfth century, in 1170 there is a record of Robert Frugardi describing surgery for goiter.
Surgical thyroidectomy was done even before the role and functions of the thyroid gland were well understood; essentially, these were historically associated with frequent postoperative hemorrhage, infections following trauma to the strap muscles and recurrent laryngeal nerves. These complications contributed to the mortality rates which was close to forty percent.
In the 19th century, thyroid surgery was considered particularly dangerous – Samuel Gross considered its approach ‘horrid butchery,’ while French medical society banned this type of surgery because of high mortality rates. Although, the chances of getting infected in the past was high due to poor and less effective surgical procedures that were used and non-use of aseptic measures. In the 1850s the surgeons applied the thyroid surgeries through different types of incisions located on the neck area, including the longitudinal and the vertical. In the year 1880, Jules Boeckel from the town of Strasbourg was the first persons to perfect the collar incision for thoracotomy, which was later widely practiced by Theodore Kocher. Kocher surgery that eliminated the death rate of thyroid surgery to 1% helped him to be honored with the Nobel Prize in 1909.
Indications
Thyroidectomy is carried out in conditions which include- benign and malignant thyroid nodules, hyperthyroidism, goiter and different types of thyroid cancer. Thyroid nodules are common, with approximately 1 % of men and 5% of women possessing this condition and 95% of which are benign nodules but 5% of which are malignant. Screening by high resolution ultrasound can identify nodules in as many as 68% of those examined especially among women and the elderly.
Localized thyroid enlargement or goiter appears to be associated with iodine deficit and is evident in about 25 percent populations in iodine deficient areas but the goiter may be autoimmune diseases in iodine sufficient areas. Some goiters or nodules are benign and would not necessarily need to be operated on. In the case of highly suspicious nodules, fine needle aspiration (FNA) is employed in biopsy. The American Thyroid Association has issued guidelines for biopsy that depends on the size and features of the nodule.
In the past, partial thyroidectomies were a common treatment for goiter but with progression in technology it is no longer required. In differentiated thyroid cancer, isotopic ablation may be adequate in cases involving small tumor while total thyroidectomy is preferred in sizable and/or high-risk malignancies.
Contraindications
Age Considerations: Depending on the age of the patient, the risk/benefit ratio of thyroid surgery can vary, and it is reasonable to discuss this with patients.
Anaplastic Thyroid Carcinoma: It is rather challenging to address this type of cancer because of its fast progression rate as well as short survival rate. Surgery can therefore be considered where complete resection is likely to be performed without complications or in the case where there is no metastasis; surgery on the other hand would still not be advisable.
Complex Surgical Factors: Other features can make outpatient thyroid surgery an issue, such as the following:
Large goiters
Extensive substernal goiter
Locally advanced cancer
Difficult hemostasis
Outcomes
In most cases, thyroidectomy is effective and provides benefits by treating illnesses such as thyroid cancer, goiter, and hyperthyroidism. In benign disease states such compression or hormonal abnormality some symptoms are relieved. Surgery can be curative in cancer where the operation is performed especially at an early stage of the illness. However, there are risks that may develop such as hypocalcemia, recurrent laryngeal nerve injury and patient’s need to take hormones for his or her entire life (if a total thyroidectomy was performed). The overall mortality is significantly low, as for the prognosis of patients with thyroid cancer is relatively good with high survival rate if adequate follow up care is is given after the operation.
Equipment
Scalpel
Metzenbaum and Mayo Scissors
Forceps
Weitlaner Retractors
Army-Navy Retractors
Harmonic Scalpel or LigaSure
Monopolar/Bipolar Cautery
Hemoclips
Suture Ligatures
Patient preparation
Preoperative Assessment for Thyroidectomy:
Medical History & Exam: Analysis of the thyroid disease of the patient and its general effect on the patient’s health status.
Blood Tests: Baseline investigations should include routine blood tests, renal and hepatic function and panel of thyroid function tests (TSH, T3, T4), calcium profile and coagulation profile.
Imaging: Ultrasound or CT scan to evaluate any changes of thyroid size and nodules.
Thyroid Function Optimization
Hyperthyroid Patients: Administer methimazole, or beta-blockers to reduce levels of the hormone.
Medication Adjustments:
Anticoagulants: The patient shall not take blood thinning drugs to avoid excessive bleeding.
Thyroid Hormone Replacement: About hypothyroid patients, the rate of therapy must be altered.
Patient Education: Therefore, it becomes important to explain the procedure, the risks that people associated with it face, and the likely outcomes that it has.
Informed Consent: Particularly, it is signed after the function has been explained to the patient.
Post-op Care: Define and describe the remedies including recovery, hormone replacement, and lifestyle alteration.
Fasting: Advise patients to avoid food intake for the next 6 to 8 hours before the time of the surgery.
Anesthesia Evaluation: Consultation with the anaesthesiologist before the surgeries.
Nerve Monitoring: An intraoperative nerve monitoring for the protection of recurrent laryngeal nerve should be initiated.
Patient position
Supine Position: The position of the patient is made to lie down in straight position also known improvised as dorsal recumbency.
Neck Extension: The neck is flexed to an extent that the thyroid gland becomes more accessible to the scissor like traction. This is usually done with the help of placing a head rest or some sort of cushion under the shoulder region enabling the head to recline back.
Head Support: When positioning the head, they can be put on a donut cushion or else fixed with tape/padding with a view of enhancing stability during surgery.

Thyroidectomy
Technique
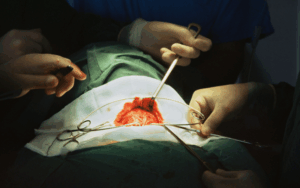
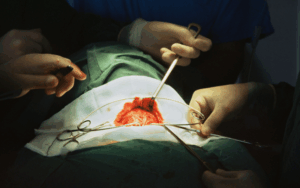
Step 1-Incision: The skin, subcutaneous tissue, fat layer and platysma are divided with a transverse incision. Skin flaps are made below the platysma and above the sternal thyroid muscle the flaps are raised up to achieve the thyroid cartilage and down to the required sternal notch.
Step 2-Strap Muscle Exposure: The sternohyoid and sternothyroid muscles are lateralised by incising the median raphe. To improve their visibility, it might be split horizontally and the nerve supply through ansa cervicalis can also be maintained.
Thyroidectomy
Step 3-Dissection: Assessment of the regional lymph nodes can be had by blunt dissection of the areolar tissue in line with the carotid sheath laterally. When it is nearly at its midpoint the Middle thyroid vein is clipped and transected. They tie and cut the superior thyroid vessels; superior thyroid artery and vein are essentially opened by applying clips, devascularized near the gland in order not to injure the superior laryngeal nerve. The inferior thyroid vein-tears after, the parathyroid glands are distinguished.
Step 4-Recurrent Laryngeal Nerve (RLN) Identification: It is found near the inferior thyroid artery and was gently separated and preserved during the procedure. The superior and the inferior parathyroid glands are then seen and kept for use in other purposes.
Step 5-Lobe Elevation: Thyroid lobe is thus displaced medially, and Berry’s ligament is incised at a little distance from the trachea. In hemithyroidectomy case, the isthmus is ligated or sectioned while in total thyroidectomy, the whole thyroid gland is resected en block.
Step 6-Hemostasis and Closure: Hemostasis is achieved and strap muscles and platysma re-suspended using absorbable sutures. The skin is closed and sometimes the drain may be left put to check on any chyle leak.
Step 7-Parathyroid Gland Preservation: Parathyroid glands that have become devascularized are replaced back into the surrounding muscles and sown with little clips to be used later in identification.
Step 8-Neck Dissection (If Necessary): Central neck dissection is done on large tumors, cases of poorly differentiated thyroid cancer or pathologic lymph nodes. Lateral neck dissection is performed for select medullary or papillary thyroid cancer.
Approach considerations
Thyroidectomy can be done in different ways depending on tumor size and extent of the thyroid disease, malignancy and patient’s health. Imaging and lab investigations carried out before surgery including ultrasound and Thyroid-stimulating hormone levels assist in establishing whether a partial or total thyroid surgery is required. The recurrent laryngeal nerve and parathyroid glands are important anatomical structures that surgeons must dissect while doing a thyroidectomy; injuries to these structures can lead to vocal cord paralysis or hypocalcemia, respectively. The tumours may be managed by minimal access surgery in cases of limited disease localized to the thyroid gland whereas the larger goitres or malignant thyroid tumours may require the traditional forms or radical surgery.
Laboratory tests
Thyroid Function Tests:
Thyroid-stimulating hormone (TSH): To measure the levels of TSH as well as thyroid hormones to know if the patient is having thyroid, hyper thyroid or hypo thyroid.
Serum TSH: To assess the facial growth in individuals with craniofacial disorders such as achondroplasia or to determine thyroid hormone levels in a hyperthyroid or hypothyroid state.
Antibody Tests:
Thyrotropin receptor antibodies (TRAb): In the evaluation of hyperthyroid patients to check for the presence or otherwise of Graves’ disease.
Thyroid peroxidase antibodies (TPO): To rule out for Hashimoto’s thyroiditis in hypothyroid patients.
Calcitonin and Carcinoembryonic Antigen (CEA): Their results support the use of science to measure tumor markers for patients with suspected or diagnosed medullary thyroid cancer.
Calcium and Parathyroid Hormone (PTH): To test the function of the parathyroid glands and to rule out of hyperparathyroidism, possible hypocalcemia or increased propensity of the same.
Genetic Testing: When certain patients have medullary thyroid cancer, they may be candidates for genetic testing for multiple endocrine neoplasia type 2(MEN2A or MEN2B).
Complications
Esophageal injury
Horner syndrome
Chyle leak
Post-surgical infection
Tracheal injury
Dysphagia

The thyroid gland has been known historically; the Romans described it as the gland with the shape of a shield. The first known reference to thyroid masses dates to the 12th and 13th centuries. From the twelfth century, in 1170 there is a record of Robert Frugardi describing surgery for goiter.
Surgical thyroidectomy was done even before the role and functions of the thyroid gland were well understood; essentially, these were historically associated with frequent postoperative hemorrhage, infections following trauma to the strap muscles and recurrent laryngeal nerves. These complications contributed to the mortality rates which was close to forty percent.
In the 19th century, thyroid surgery was considered particularly dangerous – Samuel Gross considered its approach ‘horrid butchery,’ while French medical society banned this type of surgery because of high mortality rates. Although, the chances of getting infected in the past was high due to poor and less effective surgical procedures that were used and non-use of aseptic measures. In the 1850s the surgeons applied the thyroid surgeries through different types of incisions located on the neck area, including the longitudinal and the vertical. In the year 1880, Jules Boeckel from the town of Strasbourg was the first persons to perfect the collar incision for thoracotomy, which was later widely practiced by Theodore Kocher. Kocher surgery that eliminated the death rate of thyroid surgery to 1% helped him to be honored with the Nobel Prize in 1909.
Thyroidectomy is carried out in conditions which include- benign and malignant thyroid nodules, hyperthyroidism, goiter and different types of thyroid cancer. Thyroid nodules are common, with approximately 1 % of men and 5% of women possessing this condition and 95% of which are benign nodules but 5% of which are malignant. Screening by high resolution ultrasound can identify nodules in as many as 68% of those examined especially among women and the elderly.
Localized thyroid enlargement or goiter appears to be associated with iodine deficit and is evident in about 25 percent populations in iodine deficient areas but the goiter may be autoimmune diseases in iodine sufficient areas. Some goiters or nodules are benign and would not necessarily need to be operated on. In the case of highly suspicious nodules, fine needle aspiration (FNA) is employed in biopsy. The American Thyroid Association has issued guidelines for biopsy that depends on the size and features of the nodule.
In the past, partial thyroidectomies were a common treatment for goiter but with progression in technology it is no longer required. In differentiated thyroid cancer, isotopic ablation may be adequate in cases involving small tumor while total thyroidectomy is preferred in sizable and/or high-risk malignancies.
Age Considerations: Depending on the age of the patient, the risk/benefit ratio of thyroid surgery can vary, and it is reasonable to discuss this with patients.
Anaplastic Thyroid Carcinoma: It is rather challenging to address this type of cancer because of its fast progression rate as well as short survival rate. Surgery can therefore be considered where complete resection is likely to be performed without complications or in the case where there is no metastasis; surgery on the other hand would still not be advisable.
Complex Surgical Factors: Other features can make outpatient thyroid surgery an issue, such as the following:
Large goiters
Extensive substernal goiter
Locally advanced cancer
Difficult hemostasis
In most cases, thyroidectomy is effective and provides benefits by treating illnesses such as thyroid cancer, goiter, and hyperthyroidism. In benign disease states such compression or hormonal abnormality some symptoms are relieved. Surgery can be curative in cancer where the operation is performed especially at an early stage of the illness. However, there are risks that may develop such as hypocalcemia, recurrent laryngeal nerve injury and patient’s need to take hormones for his or her entire life (if a total thyroidectomy was performed). The overall mortality is significantly low, as for the prognosis of patients with thyroid cancer is relatively good with high survival rate if adequate follow up care is is given after the operation.
Scalpel
Metzenbaum and Mayo Scissors
Forceps
Weitlaner Retractors
Army-Navy Retractors
Harmonic Scalpel or LigaSure
Monopolar/Bipolar Cautery
Hemoclips
Suture Ligatures
Preoperative Assessment for Thyroidectomy:
Medical History & Exam: Analysis of the thyroid disease of the patient and its general effect on the patient’s health status.
Blood Tests: Baseline investigations should include routine blood tests, renal and hepatic function and panel of thyroid function tests (TSH, T3, T4), calcium profile and coagulation profile.
Imaging: Ultrasound or CT scan to evaluate any changes of thyroid size and nodules.
Hyperthyroid Patients: Administer methimazole, or beta-blockers to reduce levels of the hormone.
Medication Adjustments:
Anticoagulants: The patient shall not take blood thinning drugs to avoid excessive bleeding.
Thyroid Hormone Replacement: About hypothyroid patients, the rate of therapy must be altered.
Patient Education: Therefore, it becomes important to explain the procedure, the risks that people associated with it face, and the likely outcomes that it has.
Informed Consent: Particularly, it is signed after the function has been explained to the patient.
Post-op Care: Define and describe the remedies including recovery, hormone replacement, and lifestyle alteration.
Fasting: Advise patients to avoid food intake for the next 6 to 8 hours before the time of the surgery.
Anesthesia Evaluation: Consultation with the anaesthesiologist before the surgeries.
Nerve Monitoring: An intraoperative nerve monitoring for the protection of recurrent laryngeal nerve should be initiated.
Supine Position: The position of the patient is made to lie down in straight position also known improvised as dorsal recumbency.
Neck Extension: The neck is flexed to an extent that the thyroid gland becomes more accessible to the scissor like traction. This is usually done with the help of placing a head rest or some sort of cushion under the shoulder region enabling the head to recline back.
Head Support: When positioning the head, they can be put on a donut cushion or else fixed with tape/padding with a view of enhancing stability during surgery.

Thyroidectomy
Step 1-Incision: The skin, subcutaneous tissue, fat layer and platysma are divided with a transverse incision. Skin flaps are made below the platysma and above the sternal thyroid muscle the flaps are raised up to achieve the thyroid cartilage and down to the required sternal notch.
Step 2-Strap Muscle Exposure: The sternohyoid and sternothyroid muscles are lateralised by incising the median raphe. To improve their visibility, it might be split horizontally and the nerve supply through ansa cervicalis can also be maintained.
Thyroidectomy
Step 3-Dissection: Assessment of the regional lymph nodes can be had by blunt dissection of the areolar tissue in line with the carotid sheath laterally. When it is nearly at its midpoint the Middle thyroid vein is clipped and transected. They tie and cut the superior thyroid vessels; superior thyroid artery and vein are essentially opened by applying clips, devascularized near the gland in order not to injure the superior laryngeal nerve. The inferior thyroid vein-tears after, the parathyroid glands are distinguished.
Step 4-Recurrent Laryngeal Nerve (RLN) Identification: It is found near the inferior thyroid artery and was gently separated and preserved during the procedure. The superior and the inferior parathyroid glands are then seen and kept for use in other purposes.
Step 5-Lobe Elevation: Thyroid lobe is thus displaced medially, and Berry’s ligament is incised at a little distance from the trachea. In hemithyroidectomy case, the isthmus is ligated or sectioned while in total thyroidectomy, the whole thyroid gland is resected en block.
Step 6-Hemostasis and Closure: Hemostasis is achieved and strap muscles and platysma re-suspended using absorbable sutures. The skin is closed and sometimes the drain may be left put to check on any chyle leak.
Step 7-Parathyroid Gland Preservation: Parathyroid glands that have become devascularized are replaced back into the surrounding muscles and sown with little clips to be used later in identification.
Step 8-Neck Dissection (If Necessary): Central neck dissection is done on large tumors, cases of poorly differentiated thyroid cancer or pathologic lymph nodes. Lateral neck dissection is performed for select medullary or papillary thyroid cancer.
Thyroidectomy can be done in different ways depending on tumor size and extent of the thyroid disease, malignancy and patient’s health. Imaging and lab investigations carried out before surgery including ultrasound and Thyroid-stimulating hormone levels assist in establishing whether a partial or total thyroid surgery is required. The recurrent laryngeal nerve and parathyroid glands are important anatomical structures that surgeons must dissect while doing a thyroidectomy; injuries to these structures can lead to vocal cord paralysis or hypocalcemia, respectively. The tumours may be managed by minimal access surgery in cases of limited disease localized to the thyroid gland whereas the larger goitres or malignant thyroid tumours may require the traditional forms or radical surgery.
Laboratory tests
Thyroid Function Tests:
Thyroid-stimulating hormone (TSH): To measure the levels of TSH as well as thyroid hormones to know if the patient is having thyroid, hyper thyroid or hypo thyroid.
Serum TSH: To assess the facial growth in individuals with craniofacial disorders such as achondroplasia or to determine thyroid hormone levels in a hyperthyroid or hypothyroid state.
Antibody Tests:
Thyrotropin receptor antibodies (TRAb): In the evaluation of hyperthyroid patients to check for the presence or otherwise of Graves’ disease.
Thyroid peroxidase antibodies (TPO): To rule out for Hashimoto’s thyroiditis in hypothyroid patients.
Calcitonin and Carcinoembryonic Antigen (CEA): Their results support the use of science to measure tumor markers for patients with suspected or diagnosed medullary thyroid cancer.
Calcium and Parathyroid Hormone (PTH): To test the function of the parathyroid glands and to rule out of hyperparathyroidism, possible hypocalcemia or increased propensity of the same.
Genetic Testing: When certain patients have medullary thyroid cancer, they may be candidates for genetic testing for multiple endocrine neoplasia type 2(MEN2A or MEN2B).
Complications
Esophageal injury
Horner syndrome
Chyle leak
Post-surgical infection
Tracheal injury
Dysphagia

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



