Background
Total laryngectomy is a surgical process, where the whole larynx is removed and is practiced as a treatment procedure for different types of cancer of larynx or other severe conditions of the larynx that includes trauma, radiation and unfunctional larynx.
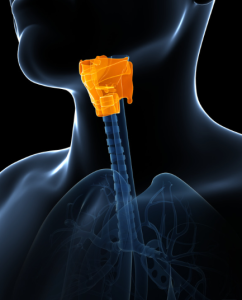
Anatomy of the larynx
This surgery radically changes the anatomy and physiology of head and neck area with major emphasis on speech, breathing and swallowing mechanisms.
Indications
Malignant diseases:
Advanced Laryngeal Cancer: Stage III or IV squamous cell carcinoma of the larynx for which chemoradiation or partial laryngectomy is not feasible.
Laryngeal cancer treated initially with radiation or chemoradiation and shows signs of recurrence.
Tumor extent that involves the larynx or invades cartilage or other structures.
Hypopharyngeal Cancer: Either when the tumor is partially or fully involves the hypopharynx and larynx, for curative purposes to control the disease.
Conservative management failure
Persistent or recurrent of cancer after Radiation therapy:
Laryngo-neoplasm surgery or methods of partial laryngectomy which is also called voice preserving surgery.
Severe laryngeal trauma: Sever injuries that alter structure and or function of the larynx including cases of laryngeal injuries or profuse fractures.
Partially denervated or rerouted upper airway that cannot be reconstructed.
Non-Malignant conditions (Rare)
Chronic Aspiration:
Unilateral aspiration leading to potentially lethal aspiration pneumonia due to irreversible failure especially in neurological diseases or congenital anatomical abnormalities.
Intractable Stenosis: Patients with end stage subglottic or glottic stenosis who do not respond to other less invasive procedures such as dilation, tracheostomy among other management strategies.
Infections: Less common, though widespread, infective illnesses, for example, laryngeal involvement in necrotizing fasciitis.
Contraindications
Inability to tolerate general anesthesia:
Severe cardiopulmonary comorbidities that make the patient unfit for surgery.
Uncontrolled or metastatic disease:
Widespread metastasis or incurable primary disease where the procedure would not improve survival or quality of life.
Severe bleeding diathesis:
Clotting abnormalities which cannot be corrected or platelet abnormalities which would represent a risk to the surgery. Unresectable tumor extension:
Invasion of the tumor into vital structures like the carotid bulb or prevertebral fascia or lymph node metastasis in the areas that cannot be surgically removed.
Severe medical comorbidities: Such comorbid conditions include heart failure where the surgery is contraindicated, severe chronic obstructive pulmonary disease or poorly controlled diabetes, etc.
Inadequate pulmonary reserve: Resection of the larynx modifies the patient’s breathing patterns; pulmonary dysfunction may worsen the postoperative period.
Outcomes
Equipment’s
Sterile surgical drapes
Suction equipment (Yankauer suction tips, tubing, canisters)
Scalpel and blades
Hemostatic instruments
Retractors
Laryngectomy set
Electrocautery or diathermy unit
Surgical sutures and staplers
Tissue scissors
Needle holders
Bone-cutting instruments (if needed)
Tracheostomy tube
Stoma protectors and dressings
Tracheal suction catheters
Voice prosthesis devices
Humidifiers and stoma cover
Electrolarynx device
Drainage systems
Monitoring devices
Surgical headlight
Sterile irrigation solutions
Patient Preparation
Preoperative Evaluation

Preoperative assessment before procedure
Medical Assessment: Patient assessment that involves general assessment of the body related to the physical condition of the patient.
Assessment of comorbid conditions such as respiratory, cardiovascular, or metabolic diseases.
Some other common investigations (complete blood count, prothrombin time, renal profile, liver function tests).
Specialist Consultations:
Oncologist: If laryngectomy is part of cancer treatment, discuss the role of surgery in the broader treatment plan.
Speech-Language Pathologist (SLP): For preoperative voice evaluation and counselling regarding communication options post-surgery.
Nutritionist: Assess nutritional status and plan for postoperative dietary needs.
Psychologist/Counsellor: Evaluate emotional well-being and provide support for coping with the life changes.
Preoperative Medical Preparation
Optimization of Health
Nutritional Support: If malnourished, consider enteral feeding (e.g., NG tube or PEG).
Smoking and Alcohol Cessation: Encourage cessation to promote healing and reduce complications.
Dental Care: Treat infections and remove problematic teeth to prevent postoperative complications.
Anesthesia and Airway Planning
Discuss Anesthesia Risks: Especially in head-and-neck cancer patients with compromised airway anatomy.
Secure Airway: In high-risk cases, plan for perioperative tracheostomy or awake intubation.
Patient Positioning
Supine Position
The patient is placed flat on their back (supine) on the operating table.
Head and Neck Positioning
The head is positioned on a headrest or gel donut, slightly extended to expose the neck fully.
A rolled towel or a shoulder roll is placed beneath the shoulders to enhance neck extension and elevate the surgical field.
Arms Position
Arms are tucked at the patient’s sides or extended on armboards, depending on the surgeon’s preference and the need for access to the surgical area.
Step 1-Preoperative Preparation
Assessment and Planning:
Thorough evaluation, imaging (CT/MRI), and endoscopy to assess tumor extent.
Preoperative discussions about outcomes, including permanent tracheostomy, loss of natural voice, and rehabilitation.
Anesthesia and Positioning:
General anesthesia is administered.
Patient is positioned supine with neck slightly extended.
Prophylactic Measures:
Prophylactic antibiotics.
Mark the incision site and tracheostomy placement.
Step 2-Incision:
A horizontal incision is typically made in the midline of the neck, just above the clavicle.
Skin flaps are elevated to expose the thyroid cartilage, cricoid cartilage, and surrounding structures.
Step 3-Exposure and Identification:
The strap muscles (sternohyoid, sternothyroid) are divided.
The thyroid gland is partially mobilized, taking care to preserve parathyroid glands and recurrent laryngeal nerves if not involved by the tumor.
Step 4-Tracheostomy:
A tracheostomy is created inferior to the larynx to secure the airway before resection.
The tracheostomy tube is inserted and secured.
Step 5-Larynx Mobilization:
The hyoid bone is dissected and freed.
The larynx is carefully mobilized from surrounding tissues, including the pharynx, prevertebral fascia, and esophagus.
Step 6-Pharyngeal Dissection:
The pharyngeal mucosa is incised circumferentially around the larynx, maintaining sufficient margins.
The surgeon takes utmost care to prevent the spillage of the tumor.
Step 7-Resection of the Larynx:
The whole larynx with its contents, including the thyroid cartilage, cricoid cartilage, and vocal cords, is excised.
Other structures like the portion of the pharynx, trachea, or base of the tongue may be included in resection if the tumor involves those areas.
Step 8-Pharyngeal Closure:
The pharyngeal defect is closed primarily using continuous sutures in order to create a watertight closure. A myocutaneous or free flap may be used if the defect is extensive.
Step 9-Neck Dissection (if indicated):
If lymph node involvement is suspected, a neck dissection may be performed simultaneously.
Step 10-Hemostasis:
Meticulous hemostasis is achieved to prevent hematoma formation.
Step 11-Drain Placement:
Suction drains are placed in the neck to manage fluid accumulation.
Step 12-Wound Closure:
The neck incision is closed in layers.
Step 13-Postoperative Management
Tracheostomy Care:
Permanent tracheostomy is managed postoperatively.
Enteral Nutrition:
Nasogastric or gastrostomy tube feeding until swallowing is restored.
Speech Rehabilitation:
Referral for voice restoration options such as esophageal speech, electrolarynx, or tracheoesophageal puncture (TEP).
Complications
Problems Related to Swallowing and Digestion
Dysphagia:
Swallowing disorder resulting from surgical procedure that interfere with the anatomical integrity of the pharynx.
Aspiration pneumonia: In case of an improper formation of the pharyngeal seal.
Nerve Damage
Accessory nerve injury: Disorders of the shoulder or weakness may occur.
Hypoglossal or vagus nerve injury: May cause tongue weakness or contralateral vocal cord paralysis.
Infection
Deep neck infections: Resulting from the spread of bacteria from the pharynx or surgical site.
Chondritis: Inflammation of the residual cartilage, especially the thyroid cartilage.
Respiratory Issues
Airway obstruction: It indicated that obstruction of the tracheostomy can occur by either swelling or secretions.
Tracheostomy complications: These are bleeding, infection, or blockage of the tracheostomy tube.
Hemorrhage Hemorrhage that occurs during surgery or afterward because of injury to large vessels of the neck, the carotid artery or the jugular veins.
Surgical Site Complications
Wound infection: Because of infection by bacteria and other microorganisms at the operation site.
Pharyngocutaneous fistula (PCF): Abnormal connection between the pharynx and skin, often due to poor healing or infection.

Total laryngectomy is a surgical process, where the whole larynx is removed and is practiced as a treatment procedure for different types of cancer of larynx or other severe conditions of the larynx that includes trauma, radiation and unfunctional larynx.
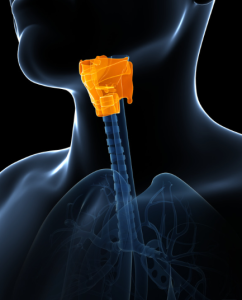
Anatomy of the larynx
This surgery radically changes the anatomy and physiology of head and neck area with major emphasis on speech, breathing and swallowing mechanisms.
Malignant diseases:
Advanced Laryngeal Cancer: Stage III or IV squamous cell carcinoma of the larynx for which chemoradiation or partial laryngectomy is not feasible.
Laryngeal cancer treated initially with radiation or chemoradiation and shows signs of recurrence.
Tumor extent that involves the larynx or invades cartilage or other structures.
Hypopharyngeal Cancer: Either when the tumor is partially or fully involves the hypopharynx and larynx, for curative purposes to control the disease.
Conservative management failure
Persistent or recurrent of cancer after Radiation therapy:
Laryngo-neoplasm surgery or methods of partial laryngectomy which is also called voice preserving surgery.
Severe laryngeal trauma: Sever injuries that alter structure and or function of the larynx including cases of laryngeal injuries or profuse fractures.
Partially denervated or rerouted upper airway that cannot be reconstructed.
Non-Malignant conditions (Rare)
Chronic Aspiration:
Unilateral aspiration leading to potentially lethal aspiration pneumonia due to irreversible failure especially in neurological diseases or congenital anatomical abnormalities.
Intractable Stenosis: Patients with end stage subglottic or glottic stenosis who do not respond to other less invasive procedures such as dilation, tracheostomy among other management strategies.
Infections: Less common, though widespread, infective illnesses, for example, laryngeal involvement in necrotizing fasciitis.
Inability to tolerate general anesthesia:
Severe cardiopulmonary comorbidities that make the patient unfit for surgery.
Uncontrolled or metastatic disease:
Widespread metastasis or incurable primary disease where the procedure would not improve survival or quality of life.
Severe bleeding diathesis:
Clotting abnormalities which cannot be corrected or platelet abnormalities which would represent a risk to the surgery. Unresectable tumor extension:
Invasion of the tumor into vital structures like the carotid bulb or prevertebral fascia or lymph node metastasis in the areas that cannot be surgically removed.
Severe medical comorbidities: Such comorbid conditions include heart failure where the surgery is contraindicated, severe chronic obstructive pulmonary disease or poorly controlled diabetes, etc.
Inadequate pulmonary reserve: Resection of the larynx modifies the patient’s breathing patterns; pulmonary dysfunction may worsen the postoperative period.
Sterile surgical drapes
Suction equipment (Yankauer suction tips, tubing, canisters)
Scalpel and blades
Hemostatic instruments
Retractors
Laryngectomy set
Electrocautery or diathermy unit
Surgical sutures and staplers
Tissue scissors
Needle holders
Bone-cutting instruments (if needed)
Tracheostomy tube
Stoma protectors and dressings
Tracheal suction catheters
Voice prosthesis devices
Humidifiers and stoma cover
Electrolarynx device
Drainage systems
Monitoring devices
Surgical headlight
Sterile irrigation solutions
Patient Preparation
Preoperative Evaluation

Preoperative assessment before procedure
Medical Assessment: Patient assessment that involves general assessment of the body related to the physical condition of the patient.
Assessment of comorbid conditions such as respiratory, cardiovascular, or metabolic diseases.
Some other common investigations (complete blood count, prothrombin time, renal profile, liver function tests).
Specialist Consultations:
Oncologist: If laryngectomy is part of cancer treatment, discuss the role of surgery in the broader treatment plan.
Speech-Language Pathologist (SLP): For preoperative voice evaluation and counselling regarding communication options post-surgery.
Nutritionist: Assess nutritional status and plan for postoperative dietary needs.
Psychologist/Counsellor: Evaluate emotional well-being and provide support for coping with the life changes.
Preoperative Medical Preparation
Optimization of Health
Nutritional Support: If malnourished, consider enteral feeding (e.g., NG tube or PEG).
Smoking and Alcohol Cessation: Encourage cessation to promote healing and reduce complications.
Dental Care: Treat infections and remove problematic teeth to prevent postoperative complications.
Anesthesia and Airway Planning
Discuss Anesthesia Risks: Especially in head-and-neck cancer patients with compromised airway anatomy.
Secure Airway: In high-risk cases, plan for perioperative tracheostomy or awake intubation.
Patient Positioning
Supine Position
The patient is placed flat on their back (supine) on the operating table.
Head and Neck Positioning
The head is positioned on a headrest or gel donut, slightly extended to expose the neck fully.
A rolled towel or a shoulder roll is placed beneath the shoulders to enhance neck extension and elevate the surgical field.
Arms Position
Arms are tucked at the patient’s sides or extended on armboards, depending on the surgeon’s preference and the need for access to the surgical area.
Assessment and Planning:
Thorough evaluation, imaging (CT/MRI), and endoscopy to assess tumor extent.
Preoperative discussions about outcomes, including permanent tracheostomy, loss of natural voice, and rehabilitation.
Anesthesia and Positioning:
General anesthesia is administered.
Patient is positioned supine with neck slightly extended.
Prophylactic Measures:
Prophylactic antibiotics.
Mark the incision site and tracheostomy placement.
Step 2-Incision:
A horizontal incision is typically made in the midline of the neck, just above the clavicle.
Skin flaps are elevated to expose the thyroid cartilage, cricoid cartilage, and surrounding structures.
Step 3-Exposure and Identification:
The strap muscles (sternohyoid, sternothyroid) are divided.
The thyroid gland is partially mobilized, taking care to preserve parathyroid glands and recurrent laryngeal nerves if not involved by the tumor.
Step 4-Tracheostomy:
A tracheostomy is created inferior to the larynx to secure the airway before resection.
The tracheostomy tube is inserted and secured.
Step 5-Larynx Mobilization:
The hyoid bone is dissected and freed.
The larynx is carefully mobilized from surrounding tissues, including the pharynx, prevertebral fascia, and esophagus.
Step 6-Pharyngeal Dissection:
The pharyngeal mucosa is incised circumferentially around the larynx, maintaining sufficient margins.
The surgeon takes utmost care to prevent the spillage of the tumor.
Step 7-Resection of the Larynx:
The whole larynx with its contents, including the thyroid cartilage, cricoid cartilage, and vocal cords, is excised.
Other structures like the portion of the pharynx, trachea, or base of the tongue may be included in resection if the tumor involves those areas.
Step 8-Pharyngeal Closure:
The pharyngeal defect is closed primarily using continuous sutures in order to create a watertight closure. A myocutaneous or free flap may be used if the defect is extensive.
Step 9-Neck Dissection (if indicated):
If lymph node involvement is suspected, a neck dissection may be performed simultaneously.
Step 10-Hemostasis:
Meticulous hemostasis is achieved to prevent hematoma formation.
Step 11-Drain Placement:
Suction drains are placed in the neck to manage fluid accumulation.
Step 12-Wound Closure:
The neck incision is closed in layers.
Step 13-Postoperative Management
Tracheostomy Care:
Permanent tracheostomy is managed postoperatively.
Enteral Nutrition:
Nasogastric or gastrostomy tube feeding until swallowing is restored.
Speech Rehabilitation:
Referral for voice restoration options such as esophageal speech, electrolarynx, or tracheoesophageal puncture (TEP).
Complications
Problems Related to Swallowing and Digestion
Dysphagia:
Swallowing disorder resulting from surgical procedure that interfere with the anatomical integrity of the pharynx.
Aspiration pneumonia: In case of an improper formation of the pharyngeal seal.
Nerve Damage
Accessory nerve injury: Disorders of the shoulder or weakness may occur.
Hypoglossal or vagus nerve injury: May cause tongue weakness or contralateral vocal cord paralysis.
Infection
Deep neck infections: Resulting from the spread of bacteria from the pharynx or surgical site.
Chondritis: Inflammation of the residual cartilage, especially the thyroid cartilage.
Respiratory Issues
Airway obstruction: It indicated that obstruction of the tracheostomy can occur by either swelling or secretions.
Tracheostomy complications: These are bleeding, infection, or blockage of the tracheostomy tube.
Hemorrhage Hemorrhage that occurs during surgery or afterward because of injury to large vessels of the neck, the carotid artery or the jugular veins.
Surgical Site Complications
Wound infection: Because of infection by bacteria and other microorganisms at the operation site.
Pharyngocutaneous fistula (PCF): Abnormal connection between the pharynx and skin, often due to poor healing or infection.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



