Background
Urography, also termed intravenous pyelography (IVP) or excretory urography (EU) is an imaging diagnostic technique to visualise human anatomy and function of the urinary system in the early 20th century.
At first, it required the administration of contrast media intravenously where these are filtered by the kidneys and excreted through the urinary system to obtain X-ray pictures of the kidneys, ureters and bladder.
The method quickly gained popularity as a non-invasive means of diagnosing urinary tract obstruction, kidney stones, ureteral tumors, congenital anomalies and other diseases of the genitourinary system. However, with advances in technology came access to more sophisticated imaging modalities such as CT and MRI. These new technologies provided better resolution, more detailed anatomical perspectives and functional information and they have gradually displaced conventional excretory urography in many clinical environments.
Indications
Excretory urography
The American College of Radiology (ACR) has outlined several accepted indications for excretory urography (EU), including:
To assess for presumed or confirmed ureteral obstruction.
Evaluating the function of the urinary tract after a trauma or an intervention, where extended cross-sectional imaging modalities are not possible or appropriate.
Exploring congenital malformations of the urinary tract in cases where other superior imaging mode are not feasible.
Scanning the urinary system for signs of hematuria or infection like a parenchymal mass or urothelial tract disease when cross-sectional imaging is unavailable.
Originally, excretory urography had been the predominant imaging technique for the urinary system. However, with the updated version of ultrasound and the growing techniques of CT and MRI based urography, the willingness to perform EU and hence expertise in it has reduced over time. However, EU is still useful in certain instances due to its dynamic imaging, ease of use, lower cost, and lower radiation dosage; it is particularly useful in the evaluation of congenital anomalies, urothelial pathology, and urinary fistulas.
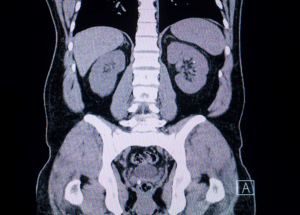
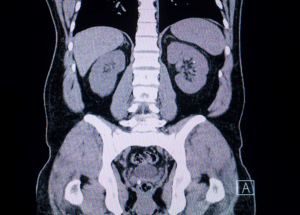
Computed tomography
Current management utilizes Computed tomography urography as the imaging modality of choice for the evaluation of the entire urinary tract and offers better detection and characterization of benign and malignant diseases. It allows for better visualisation of the lower urinary collecting system. CT scans are most useful in the evaluation of urologic tumors as it helps in localization, characterization and the stage of tumor. The indications for CT urography are quite like EU and are mainly used for assessment of the urinary collecting system in patients who present with hematuria.
Research have indicated that multidetector CT is more sensitive than EU in diagnosing Transitional cell carcinoma (TCC) of the upper urinary tract – its sensitivity being 95.8% as compared to 75%.
In the study of Abuhasanein and other authors evaluated the effectiveness of CT urography to exclude urinary bladder cancer and minimize the need for cystoscopy. This work revealed that CT urography in the corticomedullary phase yielded high accuracy in excluding bladder cancer. The negative predictive value was 99%, false negative rate 7% and false positive rate 1%.
Magnetic resonance urography
Magnetic resonance (MR) urography is mainly employed in cases of urinary tract dilatation or obstruction, especially if the use of iodinated contrast or radiation exposure is contraindicated; therefore, it is highly useful in children and pregnant women. It is less effective for detecting kidney and ureteral stones than CT but serves well for diagnosis and staging of cancers resulting from its better soft tissue contrast. MR urography has a role in the management of congenital disorders of the urogenital tract because can provide anatomical mapping. It can define vascular structures, detect any abnormalities in the urinary tract system, including hydronephrosis, in children, and provide physiological information that can minimize the use of radiation-associated techniques. A very common application is in the differentiation of normal ureteral dilation in pregnant women from obstruction.
Contraindications
Contraindications for Excretory Urography (EU)
EU is administered via an intravenous iodinated contrast material and compression devices and has contraindications connected with both. Otherwise, a confirmed pregnancy is an absolute contraindication for the use of a particular medication.
Contraindications to Iodinated Contrast Material
Allergy: Risk factors include a history of allergic reactions to contrast media or a general tendency to develop allergies.
Asthma: Patients experiencing asthma are at a higher risk for developing contrast reactions.
Cardiac Status: Patients with heart problems such as heart failure, severe cardiomyopathy, etc, there is risk associated with large volumes of contrast media.
Renal Insufficiency: These include pre-existing kidney diseases, elevated serum creatinine greater than 1.5 mg/dL, diabetes, dehydration, and specific cardiovascular diseases.
Miscellaneous: There are relative indications for patient with pheochromocytoma, sickle cell disease, multiple myeloma, especially for high osmolarity contrast medium.
Contraindications to Compression Devices
Obstruction detected on imaging.
Abdominal aortic aneurism, other intra-abdominal masses etc.
Pain in the abdominal area or surgery that has been performed in the last two weeks.
Urinary tract injury suspected during a forceful battle with a constable. If the patient has any urinary diversions or renal transplants.
CT Urography Considerations: CT urography has the same contraindications associated with the use of iodinated contrast and compression. Other are high radiation dose (14.8 mSV); hence it is contra-indicated in pregnant women and children whereby MRU may be appropriate.
Outcomes
Equipment
EU commonly called intravenous pyelography (IVP) employs conventional radiographic machines that take several pictures of the kidneys, ureters and bladder. Oblique views also assist in giving additional information especially when evaluating abnormal calcifications. Due to the better availability of the multidetector CT scanners, CT urography has been evaluated for its effectiveness as an imaging modality.
Multiple detector systems enable the isotropic volume acquisition which can be reconstructed as axial, coronal, sagittal and 3D ones. These images can be manipulated and reviewed at CT scanner workstation, stand-alone computer systems or in PACS system environment. 1.5 T machines have been investigated extensively in MR urography, while 3.0 T MR systems have been examined as well. Nevertheless, no differences in image quality have been compared between 1.5 T and 3.0 T systems and some problems might be associated with application of 3.0 T systems such as, for example, increased T1 relaxation time and higher artifacts.
While some consider essential the process of compression in the accomplishment of urographic imaging, others turn to other ways to visualize the ureters. Compression devices are available in different design; there are those that enclose the patient and others that are fixed on the exam table. Interestingly, in EU, a patient can be positioned in several ways nonetheless the patient comfort level or capabilities of the radiographic equipment.
Patient preparation
Anaesthesia
Rarely the adult patients requiring urographic procedures will require anaesthesia no matter the imaging technique chosen. On the other hand, children who need to undergo MR urography mainly need to be sedated. For this reason, several facilities engage the services of anaesthesia staff to offer these tests.
Patient position
For CT and MR urography, it is suggested that patients lie flat on their back with their hands placed above their head. This configuration assists in avoiding beam hardening artefacts in CT scans to some extent and prevents wrap-around artefacts in MR images.
Excretory urography
Step 1-Patient Preparation: Advise the patient to take one bottle of the magnesium citrate oral solution. This works as a purge to empty the bowel, thus ensuring that any renal, ureteral or bladder calcifications are not concealed by fecal matter. Inform the patient not to take any food or fluids. Make sure blood pressure and almost all laboratory results are within normal range of renal function and get the latest pregnancy test if relevant.
Step 2-Preliminary Imaging: Perform an initial KUB with a regular 14×17 inch cassette during inspiration while aligning the top edge of the cassette with the iliac crest. The radiologist also inspects the radiograph and determines the global or equivalent field of view to check whether it is sufficient and comments on calcifications.
Step 3-Contrast Injection: After the preliminary imaging is felt to be adequate, insert a peripheral intravenous line. Administer 2 x 50mL syringes of Omnipaque 300 contrast medium with force.
Step 4-Radiographs After Contrast: Perform a cone-down radiograph with the kidneys in full expiration at 1-minute post-injection. After exactly 3 minutes, KUB radiograph should be performed completely.
Excretory urography
Step 5-Compression Application: If there are no contraindications, place the patient prone on a compression paddle over the patient’s upper abdomen to provide a clear view of the renal collecting system. Following compression, obtain further anteroposterior cone-down view of the kidneys and bilateral oblique view images.
Step 6-Evaluation of Images: The radiologist goes through the images. An optimal opacification of the collecting systems should be seen, then the compression paddle is released, and a follow-up KUB radiograph is made. In some cases, a post-void cone-down radiograph of the bladder may be useful in frontal and oblique positions.
Step 7-Modification for UPJ Obstruction: When assessing patients with potential ureteropelvic junction obstruction, address them about Lasix allergy. If no prior history of allergic reaction, administer lasix at 0.5mg/kg up to 40mg given 15-20 minutes after the first contrast agent injection. Take KUB X-rays at 5, 10, and 15 min after giving Lasix’s injection. When more than 50% of the collecting system is not cleared by the 10-minute mark may indicate UPJ pathology.
CT Urography
Step 1-Pre-Examination Preparation: Patient should be advised to take sufficient fluids before the CT exam to minimize contrast induced nephropathy. A study shows that oral hydration is inexpensive and offers comparable levels of ureteral filling and contrast enhancement as IV techniques. It is also important that all the metallic objects should be avoided near the area of interest to reduce beam hardening artefacts. Place an infusion of peripheral veins before starting the examination. Place the patient in a supine position on the table with their arms raised above the head.
Step 2-Initial Imaging:
Scout Radiograph: Take a digital scout radiograph to ensure that the whole area from the diaphragm up to the iliac crest crests is covered.
Non-Contrast CT scan: Order a non-contrast CT abdomen and pelvis for the patient from the level of renal arteries to the level of the pubic symphysis using specific technical parameters including 120 KVp, dose modulated scan and 3.75 mm thickness of scan.
Step 3-Contrast Injection:
Administer 120 mL of IV contrast (or 85 mL in patients with one kidney) with a flow not exceeding 2–3 mL/sec; obtain a nephrographic phase scan after a 100-second delay.
Step 4-Post-Contrast Imaging:
Give 200 mL of saline injected after the first contrast injection as a bolus. Make the patient sit up for approximately 8 minutes to allow reabsorption of the free fluid, then lie flat to obtain a second scout radiograph. A delayed excretory phase should be acquired approximately 10 minutes after the contrast injection to demonstrate the ureters and the bladder. Produce sagittal and coronal reformation images and produce 3D volume rendered images by using a separate workstation.
Step 5-Alternative Technique (Split dose):
In patients less than 40 years old, use the ‘split dose’ procedure where a single dose of contrast is divided. Use the same technique as the standard work-up starting with a scout radiograph and non-contrast CT scan.
Administer 75 mL of a non-iodinated contrast then give a saline load of 150 mL. Wait for 8 minutes and give another 75 ml of non-iodinated contrast and 50 ml saline bolus.
Wait for approximately 100 seconds, then take the CT scan at the correct parameters.
Step 6-Data Processing: Supply volume data primarily with 0.625-mm axial slices and reformat 3.75-mm axial slices for diagnostic read by radiologist. Morrison et al, in their study, demonstrated that the single-bolus CT approach provided lower rates of repeat excretory phases and patient scan time savings for patients older than 50 years with only minimal addition of radiation dose.
Magnetic Resonance Urography
Step 1-Patient Preparation: Give IV fluids prior to the exam. Insert a urinary catheter which will facilitate the imaging process. Give diuretics during the exam to improve the assessment of the renal function.
Step 2-Imaging Protocol: Structural characterization can be done by T2-weighted images, and functional evaluations by dynamic post-contrast images. Data derived from images include contrast transit times and differential renal function.
Step 3-Early Techniques: The MR urography in the earlier years mainly relied on T2-weighted images since high signal intensity was obtained with urine. This enabled rapid imaging in any plane but only for patients who had an enlarged collecting system.
Step 4-Excretory MR Urography: Like CT urography, a gadolinium-based contrast agent is given with imaging performed in the excretory phase. Thus, low dose gadolinium is mostly administered to prevent T2 effects due to concentrated contrast in urine. Give IV diuretics to improve the study done during imaging.
Step 5-Imaging Sequences: The most basic scan is a 3D gradient echo in and out plane that suppresses fat signal. Elective breath-hold acquisitions are made to reduce the effects of motion. It is recommended to use both T1- and T2-weighted sequences in axial and coronal positions for an accurate assessment. Contrast administration follows the T2-weighted images to prevent distortion of the signal’s quality.
Step 6-Post-Contrast Imaging: The radiologist scans T2-weighted images to look for possible obstructions in the initial scans. If none is detected, an IV Lasix (furosemide) might be administered to aid in clearance. Conversely, in comprehensive study, the examination takes approximately 30-60 minutes, while singly focused study can take 15-30 minutes. Follow up imaging is performed at 3 minutes and 7 to 10 minutes post-contrast and both axial and coronal views are captured.
Step 7-Pediatric Considerations: MR urography can be performed at 1.5 T or 3 T in children and 3 T offers better image quality and detail. While 1.5 T magnets are relatively less sensitive to artifacts.
Magnetic resonance imaging
Medications and Medical devices
Furosemide: Inhibits reabsorption of sodium and chloride from the loop of Henle and distal renal tubule, leading to increased excretion of water. Excretory Urography 0.5 mg/kg IV over a maximum of 40 mg
Gadolinium-Based Contrast Agents: This class of agents causes nephrogenic systemic fibrosis (NSF) which affects dermal abnormalities and joint muscle-induced immune-driven changes in patients with renal disease. Gadolinium should be used with caution in patients with renal insufficiency due to the possibility of developing severe or even fatal complications.
Complications
Complications Related to Contrast:
IV Site Infiltration: Low volume contrast leakage generally resolves with compresses and elevation. Compartment syndrome from a leak of 30 mL or more may be considered an emergency.
Post-Procedure Care: Patients will receive a follow-up within 24 hours for increasing pain, blistering, or infection.
Nephrotoxicity: Patients with renal compromise may experience the exacerbation of their kidney failure when receiving iodinated contrast, thus labs should be run prior to imaging. These patients have been identified to suffer from nephrogenic systemic fibrosis when they are given gadolinium-based contrast.
Compression-Related Complications:
Patient Discomfort or Risk: Compression paddles can cause discomfort and in severe cases complications, especially in patients with abdominal aortic aneurysms or transplanted kidneys.
Medication

Urography, also termed intravenous pyelography (IVP) or excretory urography (EU) is an imaging diagnostic technique to visualise human anatomy and function of the urinary system in the early 20th century.
At first, it required the administration of contrast media intravenously where these are filtered by the kidneys and excreted through the urinary system to obtain X-ray pictures of the kidneys, ureters and bladder.
The method quickly gained popularity as a non-invasive means of diagnosing urinary tract obstruction, kidney stones, ureteral tumors, congenital anomalies and other diseases of the genitourinary system. However, with advances in technology came access to more sophisticated imaging modalities such as CT and MRI. These new technologies provided better resolution, more detailed anatomical perspectives and functional information and they have gradually displaced conventional excretory urography in many clinical environments.
Excretory urography
The American College of Radiology (ACR) has outlined several accepted indications for excretory urography (EU), including:
To assess for presumed or confirmed ureteral obstruction.
Evaluating the function of the urinary tract after a trauma or an intervention, where extended cross-sectional imaging modalities are not possible or appropriate.
Exploring congenital malformations of the urinary tract in cases where other superior imaging mode are not feasible.
Scanning the urinary system for signs of hematuria or infection like a parenchymal mass or urothelial tract disease when cross-sectional imaging is unavailable.
Originally, excretory urography had been the predominant imaging technique for the urinary system. However, with the updated version of ultrasound and the growing techniques of CT and MRI based urography, the willingness to perform EU and hence expertise in it has reduced over time. However, EU is still useful in certain instances due to its dynamic imaging, ease of use, lower cost, and lower radiation dosage; it is particularly useful in the evaluation of congenital anomalies, urothelial pathology, and urinary fistulas.
Computed tomography
Current management utilizes Computed tomography urography as the imaging modality of choice for the evaluation of the entire urinary tract and offers better detection and characterization of benign and malignant diseases. It allows for better visualisation of the lower urinary collecting system. CT scans are most useful in the evaluation of urologic tumors as it helps in localization, characterization and the stage of tumor. The indications for CT urography are quite like EU and are mainly used for assessment of the urinary collecting system in patients who present with hematuria.
Research have indicated that multidetector CT is more sensitive than EU in diagnosing Transitional cell carcinoma (TCC) of the upper urinary tract – its sensitivity being 95.8% as compared to 75%.
In the study of Abuhasanein and other authors evaluated the effectiveness of CT urography to exclude urinary bladder cancer and minimize the need for cystoscopy. This work revealed that CT urography in the corticomedullary phase yielded high accuracy in excluding bladder cancer. The negative predictive value was 99%, false negative rate 7% and false positive rate 1%.
Magnetic resonance urography
Magnetic resonance (MR) urography is mainly employed in cases of urinary tract dilatation or obstruction, especially if the use of iodinated contrast or radiation exposure is contraindicated; therefore, it is highly useful in children and pregnant women. It is less effective for detecting kidney and ureteral stones than CT but serves well for diagnosis and staging of cancers resulting from its better soft tissue contrast. MR urography has a role in the management of congenital disorders of the urogenital tract because can provide anatomical mapping. It can define vascular structures, detect any abnormalities in the urinary tract system, including hydronephrosis, in children, and provide physiological information that can minimize the use of radiation-associated techniques. A very common application is in the differentiation of normal ureteral dilation in pregnant women from obstruction.
Contraindications for Excretory Urography (EU)
EU is administered via an intravenous iodinated contrast material and compression devices and has contraindications connected with both. Otherwise, a confirmed pregnancy is an absolute contraindication for the use of a particular medication.
Contraindications to Iodinated Contrast Material
Allergy: Risk factors include a history of allergic reactions to contrast media or a general tendency to develop allergies.
Asthma: Patients experiencing asthma are at a higher risk for developing contrast reactions.
Cardiac Status: Patients with heart problems such as heart failure, severe cardiomyopathy, etc, there is risk associated with large volumes of contrast media.
Renal Insufficiency: These include pre-existing kidney diseases, elevated serum creatinine greater than 1.5 mg/dL, diabetes, dehydration, and specific cardiovascular diseases.
Miscellaneous: There are relative indications for patient with pheochromocytoma, sickle cell disease, multiple myeloma, especially for high osmolarity contrast medium.
Contraindications to Compression Devices
Obstruction detected on imaging.
Abdominal aortic aneurism, other intra-abdominal masses etc.
Pain in the abdominal area or surgery that has been performed in the last two weeks.
Urinary tract injury suspected during a forceful battle with a constable. If the patient has any urinary diversions or renal transplants.
CT Urography Considerations: CT urography has the same contraindications associated with the use of iodinated contrast and compression. Other are high radiation dose (14.8 mSV); hence it is contra-indicated in pregnant women and children whereby MRU may be appropriate.
EU commonly called intravenous pyelography (IVP) employs conventional radiographic machines that take several pictures of the kidneys, ureters and bladder. Oblique views also assist in giving additional information especially when evaluating abnormal calcifications. Due to the better availability of the multidetector CT scanners, CT urography has been evaluated for its effectiveness as an imaging modality.
Multiple detector systems enable the isotropic volume acquisition which can be reconstructed as axial, coronal, sagittal and 3D ones. These images can be manipulated and reviewed at CT scanner workstation, stand-alone computer systems or in PACS system environment. 1.5 T machines have been investigated extensively in MR urography, while 3.0 T MR systems have been examined as well. Nevertheless, no differences in image quality have been compared between 1.5 T and 3.0 T systems and some problems might be associated with application of 3.0 T systems such as, for example, increased T1 relaxation time and higher artifacts.
While some consider essential the process of compression in the accomplishment of urographic imaging, others turn to other ways to visualize the ureters. Compression devices are available in different design; there are those that enclose the patient and others that are fixed on the exam table. Interestingly, in EU, a patient can be positioned in several ways nonetheless the patient comfort level or capabilities of the radiographic equipment.
Patient preparation
Anaesthesia
Rarely the adult patients requiring urographic procedures will require anaesthesia no matter the imaging technique chosen. On the other hand, children who need to undergo MR urography mainly need to be sedated. For this reason, several facilities engage the services of anaesthesia staff to offer these tests.
Patient position
For CT and MR urography, it is suggested that patients lie flat on their back with their hands placed above their head. This configuration assists in avoiding beam hardening artefacts in CT scans to some extent and prevents wrap-around artefacts in MR images.
Step 1-Patient Preparation: Advise the patient to take one bottle of the magnesium citrate oral solution. This works as a purge to empty the bowel, thus ensuring that any renal, ureteral or bladder calcifications are not concealed by fecal matter. Inform the patient not to take any food or fluids. Make sure blood pressure and almost all laboratory results are within normal range of renal function and get the latest pregnancy test if relevant.
Step 2-Preliminary Imaging: Perform an initial KUB with a regular 14×17 inch cassette during inspiration while aligning the top edge of the cassette with the iliac crest. The radiologist also inspects the radiograph and determines the global or equivalent field of view to check whether it is sufficient and comments on calcifications.
Step 3-Contrast Injection: After the preliminary imaging is felt to be adequate, insert a peripheral intravenous line. Administer 2 x 50mL syringes of Omnipaque 300 contrast medium with force.
Step 4-Radiographs After Contrast: Perform a cone-down radiograph with the kidneys in full expiration at 1-minute post-injection. After exactly 3 minutes, KUB radiograph should be performed completely.
Excretory urography
Step 5-Compression Application: If there are no contraindications, place the patient prone on a compression paddle over the patient’s upper abdomen to provide a clear view of the renal collecting system. Following compression, obtain further anteroposterior cone-down view of the kidneys and bilateral oblique view images.
Step 6-Evaluation of Images: The radiologist goes through the images. An optimal opacification of the collecting systems should be seen, then the compression paddle is released, and a follow-up KUB radiograph is made. In some cases, a post-void cone-down radiograph of the bladder may be useful in frontal and oblique positions.
Step 7-Modification for UPJ Obstruction: When assessing patients with potential ureteropelvic junction obstruction, address them about Lasix allergy. If no prior history of allergic reaction, administer lasix at 0.5mg/kg up to 40mg given 15-20 minutes after the first contrast agent injection. Take KUB X-rays at 5, 10, and 15 min after giving Lasix’s injection. When more than 50% of the collecting system is not cleared by the 10-minute mark may indicate UPJ pathology.
CT Urography
Step 1-Pre-Examination Preparation: Patient should be advised to take sufficient fluids before the CT exam to minimize contrast induced nephropathy. A study shows that oral hydration is inexpensive and offers comparable levels of ureteral filling and contrast enhancement as IV techniques. It is also important that all the metallic objects should be avoided near the area of interest to reduce beam hardening artefacts. Place an infusion of peripheral veins before starting the examination. Place the patient in a supine position on the table with their arms raised above the head.
Step 2-Initial Imaging:
Scout Radiograph: Take a digital scout radiograph to ensure that the whole area from the diaphragm up to the iliac crest crests is covered.
Non-Contrast CT scan: Order a non-contrast CT abdomen and pelvis for the patient from the level of renal arteries to the level of the pubic symphysis using specific technical parameters including 120 KVp, dose modulated scan and 3.75 mm thickness of scan.
Step 3-Contrast Injection:
Administer 120 mL of IV contrast (or 85 mL in patients with one kidney) with a flow not exceeding 2–3 mL/sec; obtain a nephrographic phase scan after a 100-second delay.
Step 4-Post-Contrast Imaging:
Give 200 mL of saline injected after the first contrast injection as a bolus. Make the patient sit up for approximately 8 minutes to allow reabsorption of the free fluid, then lie flat to obtain a second scout radiograph. A delayed excretory phase should be acquired approximately 10 minutes after the contrast injection to demonstrate the ureters and the bladder. Produce sagittal and coronal reformation images and produce 3D volume rendered images by using a separate workstation.
Step 5-Alternative Technique (Split dose):
In patients less than 40 years old, use the ‘split dose’ procedure where a single dose of contrast is divided. Use the same technique as the standard work-up starting with a scout radiograph and non-contrast CT scan.
Administer 75 mL of a non-iodinated contrast then give a saline load of 150 mL. Wait for 8 minutes and give another 75 ml of non-iodinated contrast and 50 ml saline bolus.
Wait for approximately 100 seconds, then take the CT scan at the correct parameters.
Step 6-Data Processing: Supply volume data primarily with 0.625-mm axial slices and reformat 3.75-mm axial slices for diagnostic read by radiologist. Morrison et al, in their study, demonstrated that the single-bolus CT approach provided lower rates of repeat excretory phases and patient scan time savings for patients older than 50 years with only minimal addition of radiation dose.
Magnetic Resonance Urography
Step 1-Patient Preparation: Give IV fluids prior to the exam. Insert a urinary catheter which will facilitate the imaging process. Give diuretics during the exam to improve the assessment of the renal function.
Step 2-Imaging Protocol: Structural characterization can be done by T2-weighted images, and functional evaluations by dynamic post-contrast images. Data derived from images include contrast transit times and differential renal function.
Step 3-Early Techniques: The MR urography in the earlier years mainly relied on T2-weighted images since high signal intensity was obtained with urine. This enabled rapid imaging in any plane but only for patients who had an enlarged collecting system.
Step 4-Excretory MR Urography: Like CT urography, a gadolinium-based contrast agent is given with imaging performed in the excretory phase. Thus, low dose gadolinium is mostly administered to prevent T2 effects due to concentrated contrast in urine. Give IV diuretics to improve the study done during imaging.
Step 5-Imaging Sequences: The most basic scan is a 3D gradient echo in and out plane that suppresses fat signal. Elective breath-hold acquisitions are made to reduce the effects of motion. It is recommended to use both T1- and T2-weighted sequences in axial and coronal positions for an accurate assessment. Contrast administration follows the T2-weighted images to prevent distortion of the signal’s quality.
Step 6-Post-Contrast Imaging: The radiologist scans T2-weighted images to look for possible obstructions in the initial scans. If none is detected, an IV Lasix (furosemide) might be administered to aid in clearance. Conversely, in comprehensive study, the examination takes approximately 30-60 minutes, while singly focused study can take 15-30 minutes. Follow up imaging is performed at 3 minutes and 7 to 10 minutes post-contrast and both axial and coronal views are captured.
Step 7-Pediatric Considerations: MR urography can be performed at 1.5 T or 3 T in children and 3 T offers better image quality and detail. While 1.5 T magnets are relatively less sensitive to artifacts.
Magnetic resonance imaging
Furosemide: Inhibits reabsorption of sodium and chloride from the loop of Henle and distal renal tubule, leading to increased excretion of water. Excretory Urography 0.5 mg/kg IV over a maximum of 40 mg
Gadolinium-Based Contrast Agents: This class of agents causes nephrogenic systemic fibrosis (NSF) which affects dermal abnormalities and joint muscle-induced immune-driven changes in patients with renal disease. Gadolinium should be used with caution in patients with renal insufficiency due to the possibility of developing severe or even fatal complications.
Complications
Complications Related to Contrast:
IV Site Infiltration: Low volume contrast leakage generally resolves with compresses and elevation. Compartment syndrome from a leak of 30 mL or more may be considered an emergency.
Post-Procedure Care: Patients will receive a follow-up within 24 hours for increasing pain, blistering, or infection.
Nephrotoxicity: Patients with renal compromise may experience the exacerbation of their kidney failure when receiving iodinated contrast, thus labs should be run prior to imaging. These patients have been identified to suffer from nephrogenic systemic fibrosis when they are given gadolinium-based contrast.
Compression-Related Complications:
Patient Discomfort or Risk: Compression paddles can cause discomfort and in severe cases complications, especially in patients with abdominal aortic aneurysms or transplanted kidneys.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



