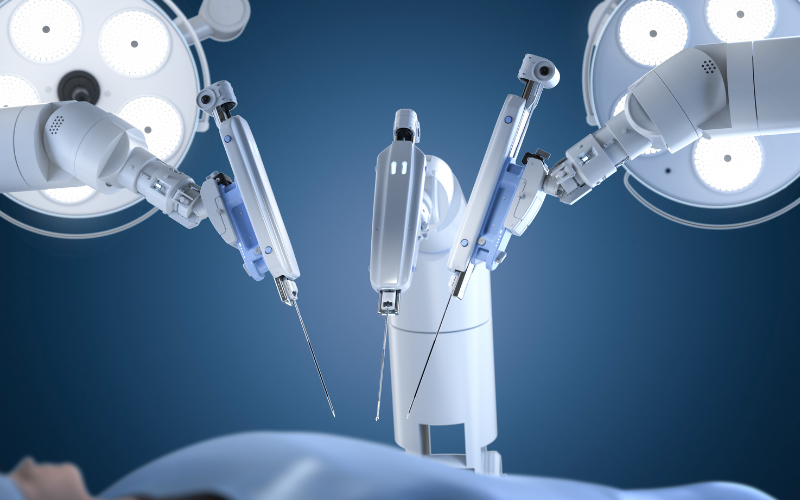
Robotic surgery has revolutionized modern surgical practice by improving ergonomic and visualization. Nevertheless, it remains geographically constrained, requiring surgeons and patients to be in the same operating room. This limitation disproportionately affects rural areas, disaster zones, and regions with limited access to specialist care. Robot-assisted surgery, a form of telesurgery, offers a potential solution by separating the physical location of the surgeon and the patient through advanced telecommunication networks.
Despite more than three decades of exploration and successful feasibility studies demonstrating the technical possibility of telesurgery, clinical evidence regarding its reliability has been limited. Most of the previous reports were single-arm or uncontrolled studies on technical success rather than patient outcomes. In order to fill this evidence gap, the first randomised controlled trial was conducted to assess whether urological telesurgery is non-inferior to the standard local robotic surgery in terms of surgical success and clinical outcome.
This multicentre, single-blind, non-inferiority randomised controlled trial was carried out in five hospitals across China from December 2023 to June 2024. Adults aged 18 to 80 years with prostate cancer or renal tumour who were scheduled for radical prostatectomy or partial nephrectomy were eligible. Patients were randomly allocated in a 1:1 ratio to either telesurgery or standard local robotic surgery. The primary outcome was the likelihood of surgical success, which was determined based on pre-specified criteria that were the completion of scheduled surgical procedures, no significant intraoperative trauma, no conversion to a different type of surgery, and no delay caused by system failure. A non-inferiority margin was set as an absolute reduction in the probability of success of 0.1.
Secondary outcomes were operational variables, perioperative complications, early recovery of the patient, oncological outcomes, workload of the medical team, and the technical work of the telesurgery system. Continuous monitoring of the technical parameters, including round-trip network latency, display latency, frame loss, and system malfunction were continuously monitored. Follow-up assessments were conducted at four and six weeks post-procedure. Primary outcome analysis used Bayesian mixed-effects logistic regression models with surgeon clustering. Both intention-to-treat and per-protocol analyses were performed.
Of the 381 patients screened, 72 were randomised, with 36 assigned to telesurgery and 36 to local surgery. Following withdrawal, 32 patients in the telesurgery group and 31 patients in the local surgery group underwent surgery. Baseline demographic and disease characteristics were well balanced between groups.
The likelihood of success of the surgery in the intention-to-treat population was 100% in the telesurgery group and 94.44% in the local surgery group. The adjusted difference in the probability of success had a 95% credible interval of (-0.03 to 0.15) and a Bayesian posterior probability of 0.99 of not being inferior. Similar results were observed in the per-protocol analysis, with a posterior probability exceeding 0.99. All credible intervals had an upper limit that exceeded the pre-specified non-inferiority margin.
Telesurgery was performed over distances ranging from 1000 km to 2800 km, with round-trip network latency between 20.1 ms and 47.5 ms. The frame loss was low, ranging from 0 to 1.5 frames per procedure. There were no occasions when telesurgery failed because of a malfunction of the system. No procedures were interrupted due to a system malfunction. Secondary outcomes, such as operative time, blood loss, complication rates, hospital stay, early recovery scores, and oncological outcomes, did not differ significantly between groups. Surgeons reported a reduced workload when performing telesurgery compared to local surgery.
This trial provides the first randomised clinical evidence that urological telesurgery is not inferior to conventional local robotic surgery regarding surgical success. Network performance was stable even over distances up to 2,800 km. Clinical outcomes, recovery, and complication rates were comparable between groups. These results suggest the potential of telesurgery to enhance the availability of expert surgical services, especially in regions with uneven medical resource distribution. Although larger studies with longer follow-up are required, this trial provides significant evidence base for the future development and clinical integration of telesurgery.
References: Wang Y, Xia D, Xu W et al. Reliability of urological telesurgery compared with local surgery: multicentre randomised controlled trial. BMJ. 2026;392:e083588. doi:10.1136/bmj-2024-083588