Sleepless and Costly: How OSA Is Hitting US and UK Workforces
March 3, 2026
Background
Severe bleeding after childbirth is known as postpartum hemorrhage which can be fatal if not timely and appropriately treated. The overdose of blood loss may result in shock. The purpose of treatment is to identify what is provoking bleeding and to stop it. This could be achieved by using embryo implantation, surgical techniques including hysterectomy or removal of placental pieces as an alternative. In order to prevent serious problems the treatment and identification of the early stage is needed. Women of any risk factors have a chance to represent postpartum hemorrhage which mediates from 1% to 10% of pregnancies and the most common takes place after the delivery.
Epidemiology
Incidence: Postpartum hemorrhage is one of the major obstetric crisis and its occurrence can vary dramatically across different regions. The next numeric fact is of interest formulated by the World Health Organization (WHO) which states that PPH happens in about 5% of all births around the world.
Geographical Variations: The percentage of PPH may trend differently between countries in the high-income category compared to those in the low-income. The areas which are endowed with poor healthcare facilities and lack adequate resources for male and female labor practitioner, as well as the quick response emergency obstetric care observe higher rates.
Pathophysiology: The mechanism of PPH involves the exposure of high volume of blood to the uterus and the placenta during normal pregnancy, which in effect makes them lacerate and ooze blood if not tightly controlled. The initial contractile process carries on until the full uterus is exposed, which reveals the placenta and the maternal blood vessels lying beneath it. Following delivery of the placenta, the uterus starts working on constriction, which is closing the veins that feed it and triggering at the same moment.
Anatomy
Pathophysiology
The pathophysiology of postpartum hemorrhage (PPH) involves disruptions in the normal physiological processes that occur during and after childbirth, leading to excessive bleeding. PPH is typically categorized into primary and secondary types based on the timing of onset.
Etiology
Postpartum hemorrhage (PPH) can have several causes but the most frequent one is uterine atony and which occurs when the uterus is unable to shrink and retract after giving birth which results in profuse bleeding.
Genetics
Prognostic Factors
The prognostic factors of postpartum hemorrhage are highly relevant to identify who is at a higher risk treatment and management of disease and mother’s outcomes improvement. The existing ones are not designed to be utilized in medicine.
Clinical History
Age group: Inadequate prenatal care, immature reproductive systems, and lack of identifying difficulties may cause to young women in their late twenties and early thirties to become an easy preys to premature pregnancies (PPH). Teenage mothers are also most likely to experience preterm labor, multiparity, and other obstetrics related problems. There might be an increased risk of getting sick among the older women.
Physical Examination
Assessing uterine tone and size: Uses a hand resting on the fundus and palpating the anterior wall of the uterus.
Inspecting for retained placenta or clots: If the placenta has been delivered, inspect for retained portions. If undelivered or clots are distending the uterus, manual exploration and removal are necessary.
Examining for cervical and vaginal lacerations: These may be palpated.
Inspecting for hematomas: Palpation and inspection may reveal hematomas requiring treatment.
Visualizing the lower genital tract: If uterine atony has been controlled, it may reveal bleeding sites.
Age group
Associated comorbidity
Comorbidities: Type 2 diabetes, coagulation problems, and hypertension can all raise the possibility of PPH. Women who are currently experiencing medical problems may be more susceptible to problems during pregnancy and after giving birth. Activities: PPH can be caused by trauma or damage sustained during delivery, particularly in instances of emergency cesarean sections or instrumental births. Women who are physically active or who have had uterus surgery in the past may be more vulnerable.
Associated activity
Acuity of presentation
Immediate Postpartum Period: The blood loss occurred most commonly during the first 24 hours after labor suspension for primary PPH. Severe cases of ectopic pregnancy that breach the fallopian tube might be accompanied by signs of shock, for instance, tachycardia and low blood pressure. Additionally, women will experience profuse vaginal bleeding as well as a shockingly large uterus.
Delayed Postpartum Period: Aside from the first 24 hours and a few more weeks that are after giving birth, during such period secondary PPH is also possible. The beginning of the disease is gradually developing and is indicated by apathy, anemia, abnormal bleeding, as well as recurrent infections which may deteriorate to a crisis.
Severe Acuity: Hemorrhagic shock as a volume deficit state where rapid and significant blood loss might be encountered in dramatic scenarios is a possible outcome. These are some of the symptoms including, slow or fast pulse, cold and clammy skin, marked breathing, and change of mental status.
Differential Diagnoses
Lacerations: There may be tears of the cervix, of the vagina, or of the perineum which will cause hemorrhaging in some of the most extreme situations.
Uterine inversion: This condition of complicated nature is though uncommon but still particular in which an uterus goes inside out facing the risk of severe bleeding.
Retained placenta: The retained parts might cause bleeding if left unnoticed in uterus.
Coagulation disorders: Abnormalities in Coagulation which is the blood thinning process increase the chance of the bleeding.
Placenta accreta: Placental harboring reaches adhesive depth of uterus layers, which gives high probability of bleeding to occur.
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
Initial Assessment and Stabilization for Postpartum Bleeding
Uterine Massage: Stimulate contractions and control uterine atony.
Uterotonic Medications: Administer uterotonic agents to promote uterine contractions.
Bimanual Compression: Considered for persistent bleeding.
Uterine Tamponade: Used for persistent bleeding.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Coagulopathy Management: Administer blood products, clotting factors, or specific reversal agents to address coagulopathies.
Interventional Radiology Procedures: Uterine artery embolisation is one interventional radiology treatment that may be explored in situations of chronic bleeding.
Intrauterine Balloon Tamponade: Placement of a balloon device in the uterus can help control bleeding by applying pressure to the uterine walls.
Continued Monitoring: Continuous monitoring of vital signs, laboratory parameters, and urine output to assess the response to interventions and detect any recurrence of bleeding.
Maternal Resuscitation: Ongoing support for maternal well-being, including correction of electrolyte imbalances and organ perfusion.
Psychological Support: Provide emotional support to the patient and involve mental health professionals as needed.
Post-Treatment Monitoring: Close monitoring in the postpartum period to identify and address any ongoing complications.
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
use-of-a-non-pharmacological-approach-for-treating-postpartum-hemorrhage
Cervical Massage: A gentle massage of the cervix is a useful method to counter the cervix tension and decrease the bleeding. This period, therefore, helps to control and flush out the blood out from the womb which leads to bleeding.
Uterine Compression: Utus massaging is done mainly to control bleeding. Here, you just have to put your hand on the womb; press on it slightly to stop the bleeding.
Bimanual Uterine Compression: This exerting handles pressure with thumbs and fingers. Either one or both hands are inserted into the uterus to press against the uterus using one hand while the other hand is used on the abdomen for extra pressure.
Uterine Dressings: Otherwise bleeding is needed to be cauterized by means of using gauze or any other absorbent material inserted into the uterus. It must be done carefully in order to check the minimal damage because of possible sensitivity of the organ.
Balloon Tamponade: In this method, an inflated balloon catheter is introduced inside the uterus and then it is inflated to exert the on the blood clotting and wall of the uterus. Sometimes commercial devices such as Bakri or Sengstaken-Blakemore tubes can be used for this purpose.
Role of oxytocin in the treatment of Postpartum hemorrhage
The existence of maternal complications and deaths in postpartum period has a great deal to do with PPH. The uterine contractions that are triggered by oxytocin, which is a hormone, improve the uterus from bleeding excessively and reduces the possibility of hemorrhage from occurring. It is aimed at stopping the uterus from failing to contract efficiently after delivery which is otherwise called uterine atonia (in Greek). Along with it occasionally being administered as a preventative measure, oxytocin is one of the most commonly used anesthetics.It is usually given at the third phase of labor to stop excessive bleeding. Another oxytocin analog that promotes contractions and lessens postpartum hemorrhage is carbetocin, particularly when oxytocin is neither practical or efficient.
Role of Ergot alkaloids in controlling excessive bleeding
The alkaloids of ergot species (also known as methylerzometrine and ergometrine) are absolutely essential for the treatment of postpartum bleeding (PPB) due to their ability to ensure violent contractions of the smooth muscle, including the uterus. Through the process of uterine muscle contraction, the blood vessels that are on the uterus wall will become narrow, hence reducing the amount of blood that will be spilled out. And after labor they will likely receive an IV or IM injection.
Methylergometrine/Methyergonovine: Ergonovine, is the other drug which can cause complications. It is a member of the ergot class of the ergot alkaloids that produces labor contractions in smooth muscle, particularly in smooth muscle of the uterus. Methylergometrine is a drug which assists in treating and preventing of uterine atony by helping in term of constricting the uterine muscles.
Ergometrine: The ergot alkaloid ergometrine recently grouped as the ergovine, does very important postpartum hemorrhage (PPH) treatment. Ergometrine is used in a similar manner to control a possibly excessive bleed after delivery, which is achieved by mechanism of action on smooth muscle, specifically, the uterine tissue muscle. The ivermectin drug given against parasitic infections is almost always administered intravenously (IV) or intramuscularly (IM). For the current treatment guidelines, many uterotonic drugs and therapy options are employed along with it. Post-partum hemorrhage protocols are among the regimes where this drug is a frequent, or first-line therapy.
Role of prostaglandins
Enzymatic inhibitor (prostaglandins) is one of the active ingredients of the therapy of PPH. These include proteins and other substances manufacturing in different organ tissues, such as reproductive organs. The influence on physiological functions is diverse. Prostaglandins, especially some of them, e.g. misoprostol (a misoprostol analogue of prostaglandin E1), can provoke strong uterine contractions (among the prostaglandin types). This is precisely what is required in the postpartum phase as a pre-emptive measure to avoid any bleeding complications. The uterus should contract, giving control to the bleeding. The inefficiency of the uterine to contract following childbirth is the notable cause of postpartum haemorrhage which is a uterine atony. Prostaglandins therefore can be given as a supplemental dose in organic response to uterine atony, thus preventing the progress of any moments.
Misoprostol: It is a synthanalog of progestagenetob compound that is widely applied in the treatment of postpartum hemorrhage. It is commonly attributed with oral or rectal routes of administrations and constitutes one of a few choices.
Carboprost: It is achieved by induction of the uterine contraction which results in raising tone and reducing the menstrual blood loss. It moreover induce the uterus softening and dilatation. The first use of which is to manage uterine atonia (reflux of bleeding) after childbirth since failed uterine contractions lead to bleeding.
use-of-intervention-with-a-procedure-in-treating-postpartum-hemorrhage
Uterine Massage and Compression: Dominating uterine massaging requires a physician or a midwife to apply pressure to the top of the uterus to be able to stimulate contractions that help control postpartum bleeding. This can also be done using uterine compression techniques such as bimanual compression or a uterine balloon enclosing. These are used to add additional pressure and help gain control over bleeding.
Uterotonics: Usually, oxytocin and other types of uterotonic medications are obtained initially to give contracting for the uterus by stimulating them. If the previous step is ineffective, administrating misoprostol, methylergonovine, and, or carboprost may be included in the next steps.
Uterine Artery Embolization (UAE): UAE has many similarities to sling procedure. The filling of space between uterine arteries with tiny particles is mean to stop of blood flow and decrease of uterine haemorrhage. It is a gangster-proof mode. It is many times be used when all the available treatment modalities including medical management and surgery are not desirable or are not offering an immediate relief.
Selective Arterial Embolization: Complications of postpartum hemorrhage can be reduced significantly with appropriate treatment of vascular anomalies or trauma, and options that may be considered are selective arterial embolizations. This can be carried out with the procedure of emulsion agents into the very branches of arteries, which are the source of bleeding.
B-Lynch Suture: Placement of a compression suture around the uterus that controls bleeding is the laparoscopic approach that is used during this surgery. One of its main utility is during uterine atony.
Hysterectomy: In severe clinical cases where conservative treatments (employing drugs, medications and other efforts) do not stop the bleeding, uterus may be removed hence hysterectomy (surgical procedure that involves removal of uterus) can be performed. This is a decisive (or concrete) intervention, and normally, it is considered as a last possible solution after everything else has been tried.
use-of-phases-in-managing-postpartum-hemorrhage
Antenatal care, determining appropriate treatment methods for the final stage of labor labor, and conducting a reliable uterine examination all can assist with the prevention of postpartum hemorrhage. The use of utrotonic drugs and massage to prevent uterine atony can be supplemented by means of compression. Further medication may also be used in cases where previous treatments were ineffective. To cure hypovolemia, fluids can be administered intravenously, and blood transfusions can be given. Two minimally invasive treatments in vogue are selective arterial embolization and uterine artery embolization (UAE). Uterine excision, laparotomy as an exploratory diagnostic, and B-Lynch sutures form the surgical treatment.
Medication
(off-label):
600 mcg orally within one minute of delivery as prophylaxis
800 mcg orally once as treatment
Administer 0.2mg intramuscularly or intravenously every 2 to 4 hours whenever necessary, then administer 0.2 to 0.4mg orally every 6 to 8 hours whenever necessary for 2 to 7 days.
Do not exceed more than 5 doses.
Due to the risk of hypertension and cerebrovascular accident, only administer intravenously in an emergency.
Monitor blood pressure for more than one minute after administration.
Refractory Cluster Headache (Off-label)
Administer 0.2 mg orally thrice or four times a day. Do not continue for more than 6 months.
Administer 100mcg intravenously or intramuscularly for vaginal delivery.
Administer 100mcg intravenously for cesarean delivery.
Intramuscularly administer 200 to 500 micrograms of ergometrine following placental expulsion or when bleeding occurs;
In emergency situations, ergometrine may be administered intravenously at a dosage ranging from 250 to 500 micrograms
Dose Adjustments
N/A
Intravenous (IV)
1 g in 10 mL (100 mg/mL) Intravenous (IV) at 1 ml/minute (i.e., given over 10 minutes)
If bleeding does not stop after 30 minutes or if bleeding starts again within 24 hours of finishing the first dose, another 1 g IV dose will be given
0.2 mg intramuscular/intravenous every 2 to 4hours when necessary; should not exceed more than 5 doses, following 0.2 to 0.4 mg orally every 3-4 times a day when necessary for 2 to 7 days
Administer intravenous only incase of emergency for Hypertension and CVA
Administer more than 1 minute & monitor Blood pressure
Future Trends
References
Severe bleeding after childbirth is known as postpartum hemorrhage which can be fatal if not timely and appropriately treated. The overdose of blood loss may result in shock. The purpose of treatment is to identify what is provoking bleeding and to stop it. This could be achieved by using embryo implantation, surgical techniques including hysterectomy or removal of placental pieces as an alternative. In order to prevent serious problems the treatment and identification of the early stage is needed. Women of any risk factors have a chance to represent postpartum hemorrhage which mediates from 1% to 10% of pregnancies and the most common takes place after the delivery.
Incidence: Postpartum hemorrhage is one of the major obstetric crisis and its occurrence can vary dramatically across different regions. The next numeric fact is of interest formulated by the World Health Organization (WHO) which states that PPH happens in about 5% of all births around the world.
Geographical Variations: The percentage of PPH may trend differently between countries in the high-income category compared to those in the low-income. The areas which are endowed with poor healthcare facilities and lack adequate resources for male and female labor practitioner, as well as the quick response emergency obstetric care observe higher rates.
Pathophysiology: The mechanism of PPH involves the exposure of high volume of blood to the uterus and the placenta during normal pregnancy, which in effect makes them lacerate and ooze blood if not tightly controlled. The initial contractile process carries on until the full uterus is exposed, which reveals the placenta and the maternal blood vessels lying beneath it. Following delivery of the placenta, the uterus starts working on constriction, which is closing the veins that feed it and triggering at the same moment.
The pathophysiology of postpartum hemorrhage (PPH) involves disruptions in the normal physiological processes that occur during and after childbirth, leading to excessive bleeding. PPH is typically categorized into primary and secondary types based on the timing of onset.
Postpartum hemorrhage (PPH) can have several causes but the most frequent one is uterine atony and which occurs when the uterus is unable to shrink and retract after giving birth which results in profuse bleeding.
The prognostic factors of postpartum hemorrhage are highly relevant to identify who is at a higher risk treatment and management of disease and mother’s outcomes improvement. The existing ones are not designed to be utilized in medicine.
Age group: Inadequate prenatal care, immature reproductive systems, and lack of identifying difficulties may cause to young women in their late twenties and early thirties to become an easy preys to premature pregnancies (PPH). Teenage mothers are also most likely to experience preterm labor, multiparity, and other obstetrics related problems. There might be an increased risk of getting sick among the older women.
Assessing uterine tone and size: Uses a hand resting on the fundus and palpating the anterior wall of the uterus.
Inspecting for retained placenta or clots: If the placenta has been delivered, inspect for retained portions. If undelivered or clots are distending the uterus, manual exploration and removal are necessary.
Examining for cervical and vaginal lacerations: These may be palpated.
Inspecting for hematomas: Palpation and inspection may reveal hematomas requiring treatment.
Visualizing the lower genital tract: If uterine atony has been controlled, it may reveal bleeding sites.
Comorbidities: Type 2 diabetes, coagulation problems, and hypertension can all raise the possibility of PPH. Women who are currently experiencing medical problems may be more susceptible to problems during pregnancy and after giving birth. Activities: PPH can be caused by trauma or damage sustained during delivery, particularly in instances of emergency cesarean sections or instrumental births. Women who are physically active or who have had uterus surgery in the past may be more vulnerable.
Immediate Postpartum Period: The blood loss occurred most commonly during the first 24 hours after labor suspension for primary PPH. Severe cases of ectopic pregnancy that breach the fallopian tube might be accompanied by signs of shock, for instance, tachycardia and low blood pressure. Additionally, women will experience profuse vaginal bleeding as well as a shockingly large uterus.
Delayed Postpartum Period: Aside from the first 24 hours and a few more weeks that are after giving birth, during such period secondary PPH is also possible. The beginning of the disease is gradually developing and is indicated by apathy, anemia, abnormal bleeding, as well as recurrent infections which may deteriorate to a crisis.
Severe Acuity: Hemorrhagic shock as a volume deficit state where rapid and significant blood loss might be encountered in dramatic scenarios is a possible outcome. These are some of the symptoms including, slow or fast pulse, cold and clammy skin, marked breathing, and change of mental status.
Lacerations: There may be tears of the cervix, of the vagina, or of the perineum which will cause hemorrhaging in some of the most extreme situations.
Uterine inversion: This condition of complicated nature is though uncommon but still particular in which an uterus goes inside out facing the risk of severe bleeding.
Retained placenta: The retained parts might cause bleeding if left unnoticed in uterus.
Coagulation disorders: Abnormalities in Coagulation which is the blood thinning process increase the chance of the bleeding.
Placenta accreta: Placental harboring reaches adhesive depth of uterus layers, which gives high probability of bleeding to occur.
Initial Assessment and Stabilization for Postpartum Bleeding
Uterine Massage: Stimulate contractions and control uterine atony.
Uterotonic Medications: Administer uterotonic agents to promote uterine contractions.
Bimanual Compression: Considered for persistent bleeding.
Uterine Tamponade: Used for persistent bleeding.
Coagulopathy Management: Administer blood products, clotting factors, or specific reversal agents to address coagulopathies.
Interventional Radiology Procedures: Uterine artery embolisation is one interventional radiology treatment that may be explored in situations of chronic bleeding.
Intrauterine Balloon Tamponade: Placement of a balloon device in the uterus can help control bleeding by applying pressure to the uterine walls.
Continued Monitoring: Continuous monitoring of vital signs, laboratory parameters, and urine output to assess the response to interventions and detect any recurrence of bleeding.
Maternal Resuscitation: Ongoing support for maternal well-being, including correction of electrolyte imbalances and organ perfusion.
Psychological Support: Provide emotional support to the patient and involve mental health professionals as needed.
Post-Treatment Monitoring: Close monitoring in the postpartum period to identify and address any ongoing complications.
OB/GYN and Women\'s Health
Cervical Massage: A gentle massage of the cervix is a useful method to counter the cervix tension and decrease the bleeding. This period, therefore, helps to control and flush out the blood out from the womb which leads to bleeding.
Uterine Compression: Utus massaging is done mainly to control bleeding. Here, you just have to put your hand on the womb; press on it slightly to stop the bleeding.
Bimanual Uterine Compression: This exerting handles pressure with thumbs and fingers. Either one or both hands are inserted into the uterus to press against the uterus using one hand while the other hand is used on the abdomen for extra pressure.
Uterine Dressings: Otherwise bleeding is needed to be cauterized by means of using gauze or any other absorbent material inserted into the uterus. It must be done carefully in order to check the minimal damage because of possible sensitivity of the organ.
Balloon Tamponade: In this method, an inflated balloon catheter is introduced inside the uterus and then it is inflated to exert the on the blood clotting and wall of the uterus. Sometimes commercial devices such as Bakri or Sengstaken-Blakemore tubes can be used for this purpose.
OB/GYN and Women\'s Health
The existence of maternal complications and deaths in postpartum period has a great deal to do with PPH. The uterine contractions that are triggered by oxytocin, which is a hormone, improve the uterus from bleeding excessively and reduces the possibility of hemorrhage from occurring. It is aimed at stopping the uterus from failing to contract efficiently after delivery which is otherwise called uterine atonia (in Greek). Along with it occasionally being administered as a preventative measure, oxytocin is one of the most commonly used anesthetics.It is usually given at the third phase of labor to stop excessive bleeding. Another oxytocin analog that promotes contractions and lessens postpartum hemorrhage is carbetocin, particularly when oxytocin is neither practical or efficient.
OB/GYN and Women\'s Health
The alkaloids of ergot species (also known as methylerzometrine and ergometrine) are absolutely essential for the treatment of postpartum bleeding (PPB) due to their ability to ensure violent contractions of the smooth muscle, including the uterus. Through the process of uterine muscle contraction, the blood vessels that are on the uterus wall will become narrow, hence reducing the amount of blood that will be spilled out. And after labor they will likely receive an IV or IM injection.
Methylergometrine/Methyergonovine: Ergonovine, is the other drug which can cause complications. It is a member of the ergot class of the ergot alkaloids that produces labor contractions in smooth muscle, particularly in smooth muscle of the uterus. Methylergometrine is a drug which assists in treating and preventing of uterine atony by helping in term of constricting the uterine muscles.
Ergometrine: The ergot alkaloid ergometrine recently grouped as the ergovine, does very important postpartum hemorrhage (PPH) treatment. Ergometrine is used in a similar manner to control a possibly excessive bleed after delivery, which is achieved by mechanism of action on smooth muscle, specifically, the uterine tissue muscle. The ivermectin drug given against parasitic infections is almost always administered intravenously (IV) or intramuscularly (IM). For the current treatment guidelines, many uterotonic drugs and therapy options are employed along with it. Post-partum hemorrhage protocols are among the regimes where this drug is a frequent, or first-line therapy.
Enzymatic inhibitor (prostaglandins) is one of the active ingredients of the therapy of PPH. These include proteins and other substances manufacturing in different organ tissues, such as reproductive organs. The influence on physiological functions is diverse. Prostaglandins, especially some of them, e.g. misoprostol (a misoprostol analogue of prostaglandin E1), can provoke strong uterine contractions (among the prostaglandin types). This is precisely what is required in the postpartum phase as a pre-emptive measure to avoid any bleeding complications. The uterus should contract, giving control to the bleeding. The inefficiency of the uterine to contract following childbirth is the notable cause of postpartum haemorrhage which is a uterine atony. Prostaglandins therefore can be given as a supplemental dose in organic response to uterine atony, thus preventing the progress of any moments.
Misoprostol: It is a synthanalog of progestagenetob compound that is widely applied in the treatment of postpartum hemorrhage. It is commonly attributed with oral or rectal routes of administrations and constitutes one of a few choices.
Carboprost: It is achieved by induction of the uterine contraction which results in raising tone and reducing the menstrual blood loss. It moreover induce the uterus softening and dilatation. The first use of which is to manage uterine atonia (reflux of bleeding) after childbirth since failed uterine contractions lead to bleeding.
OB/GYN and Women\'s Health
Uterine Massage and Compression: Dominating uterine massaging requires a physician or a midwife to apply pressure to the top of the uterus to be able to stimulate contractions that help control postpartum bleeding. This can also be done using uterine compression techniques such as bimanual compression or a uterine balloon enclosing. These are used to add additional pressure and help gain control over bleeding.
Uterotonics: Usually, oxytocin and other types of uterotonic medications are obtained initially to give contracting for the uterus by stimulating them. If the previous step is ineffective, administrating misoprostol, methylergonovine, and, or carboprost may be included in the next steps.
Uterine Artery Embolization (UAE): UAE has many similarities to sling procedure. The filling of space between uterine arteries with tiny particles is mean to stop of blood flow and decrease of uterine haemorrhage. It is a gangster-proof mode. It is many times be used when all the available treatment modalities including medical management and surgery are not desirable or are not offering an immediate relief.
Selective Arterial Embolization: Complications of postpartum hemorrhage can be reduced significantly with appropriate treatment of vascular anomalies or trauma, and options that may be considered are selective arterial embolizations. This can be carried out with the procedure of emulsion agents into the very branches of arteries, which are the source of bleeding.
B-Lynch Suture: Placement of a compression suture around the uterus that controls bleeding is the laparoscopic approach that is used during this surgery. One of its main utility is during uterine atony.
Hysterectomy: In severe clinical cases where conservative treatments (employing drugs, medications and other efforts) do not stop the bleeding, uterus may be removed hence hysterectomy (surgical procedure that involves removal of uterus) can be performed. This is a decisive (or concrete) intervention, and normally, it is considered as a last possible solution after everything else has been tried.
OB/GYN and Women\'s Health
Antenatal care, determining appropriate treatment methods for the final stage of labor labor, and conducting a reliable uterine examination all can assist with the prevention of postpartum hemorrhage. The use of utrotonic drugs and massage to prevent uterine atony can be supplemented by means of compression. Further medication may also be used in cases where previous treatments were ineffective. To cure hypovolemia, fluids can be administered intravenously, and blood transfusions can be given. Two minimally invasive treatments in vogue are selective arterial embolization and uterine artery embolization (UAE). Uterine excision, laparotomy as an exploratory diagnostic, and B-Lynch sutures form the surgical treatment.
Severe bleeding after childbirth is known as postpartum hemorrhage which can be fatal if not timely and appropriately treated. The overdose of blood loss may result in shock. The purpose of treatment is to identify what is provoking bleeding and to stop it. This could be achieved by using embryo implantation, surgical techniques including hysterectomy or removal of placental pieces as an alternative. In order to prevent serious problems the treatment and identification of the early stage is needed. Women of any risk factors have a chance to represent postpartum hemorrhage which mediates from 1% to 10% of pregnancies and the most common takes place after the delivery.
Incidence: Postpartum hemorrhage is one of the major obstetric crisis and its occurrence can vary dramatically across different regions. The next numeric fact is of interest formulated by the World Health Organization (WHO) which states that PPH happens in about 5% of all births around the world.
Geographical Variations: The percentage of PPH may trend differently between countries in the high-income category compared to those in the low-income. The areas which are endowed with poor healthcare facilities and lack adequate resources for male and female labor practitioner, as well as the quick response emergency obstetric care observe higher rates.
Pathophysiology: The mechanism of PPH involves the exposure of high volume of blood to the uterus and the placenta during normal pregnancy, which in effect makes them lacerate and ooze blood if not tightly controlled. The initial contractile process carries on until the full uterus is exposed, which reveals the placenta and the maternal blood vessels lying beneath it. Following delivery of the placenta, the uterus starts working on constriction, which is closing the veins that feed it and triggering at the same moment.
The pathophysiology of postpartum hemorrhage (PPH) involves disruptions in the normal physiological processes that occur during and after childbirth, leading to excessive bleeding. PPH is typically categorized into primary and secondary types based on the timing of onset.
Postpartum hemorrhage (PPH) can have several causes but the most frequent one is uterine atony and which occurs when the uterus is unable to shrink and retract after giving birth which results in profuse bleeding.
The prognostic factors of postpartum hemorrhage are highly relevant to identify who is at a higher risk treatment and management of disease and mother’s outcomes improvement. The existing ones are not designed to be utilized in medicine.
Age group: Inadequate prenatal care, immature reproductive systems, and lack of identifying difficulties may cause to young women in their late twenties and early thirties to become an easy preys to premature pregnancies (PPH). Teenage mothers are also most likely to experience preterm labor, multiparity, and other obstetrics related problems. There might be an increased risk of getting sick among the older women.
Assessing uterine tone and size: Uses a hand resting on the fundus and palpating the anterior wall of the uterus.
Inspecting for retained placenta or clots: If the placenta has been delivered, inspect for retained portions. If undelivered or clots are distending the uterus, manual exploration and removal are necessary.
Examining for cervical and vaginal lacerations: These may be palpated.
Inspecting for hematomas: Palpation and inspection may reveal hematomas requiring treatment.
Visualizing the lower genital tract: If uterine atony has been controlled, it may reveal bleeding sites.
Comorbidities: Type 2 diabetes, coagulation problems, and hypertension can all raise the possibility of PPH. Women who are currently experiencing medical problems may be more susceptible to problems during pregnancy and after giving birth. Activities: PPH can be caused by trauma or damage sustained during delivery, particularly in instances of emergency cesarean sections or instrumental births. Women who are physically active or who have had uterus surgery in the past may be more vulnerable.
Immediate Postpartum Period: The blood loss occurred most commonly during the first 24 hours after labor suspension for primary PPH. Severe cases of ectopic pregnancy that breach the fallopian tube might be accompanied by signs of shock, for instance, tachycardia and low blood pressure. Additionally, women will experience profuse vaginal bleeding as well as a shockingly large uterus.
Delayed Postpartum Period: Aside from the first 24 hours and a few more weeks that are after giving birth, during such period secondary PPH is also possible. The beginning of the disease is gradually developing and is indicated by apathy, anemia, abnormal bleeding, as well as recurrent infections which may deteriorate to a crisis.
Severe Acuity: Hemorrhagic shock as a volume deficit state where rapid and significant blood loss might be encountered in dramatic scenarios is a possible outcome. These are some of the symptoms including, slow or fast pulse, cold and clammy skin, marked breathing, and change of mental status.
Lacerations: There may be tears of the cervix, of the vagina, or of the perineum which will cause hemorrhaging in some of the most extreme situations.
Uterine inversion: This condition of complicated nature is though uncommon but still particular in which an uterus goes inside out facing the risk of severe bleeding.
Retained placenta: The retained parts might cause bleeding if left unnoticed in uterus.
Coagulation disorders: Abnormalities in Coagulation which is the blood thinning process increase the chance of the bleeding.
Placenta accreta: Placental harboring reaches adhesive depth of uterus layers, which gives high probability of bleeding to occur.
Initial Assessment and Stabilization for Postpartum Bleeding
Uterine Massage: Stimulate contractions and control uterine atony.
Uterotonic Medications: Administer uterotonic agents to promote uterine contractions.
Bimanual Compression: Considered for persistent bleeding.
Uterine Tamponade: Used for persistent bleeding.
Coagulopathy Management: Administer blood products, clotting factors, or specific reversal agents to address coagulopathies.
Interventional Radiology Procedures: Uterine artery embolisation is one interventional radiology treatment that may be explored in situations of chronic bleeding.
Intrauterine Balloon Tamponade: Placement of a balloon device in the uterus can help control bleeding by applying pressure to the uterine walls.
Continued Monitoring: Continuous monitoring of vital signs, laboratory parameters, and urine output to assess the response to interventions and detect any recurrence of bleeding.
Maternal Resuscitation: Ongoing support for maternal well-being, including correction of electrolyte imbalances and organ perfusion.
Psychological Support: Provide emotional support to the patient and involve mental health professionals as needed.
Post-Treatment Monitoring: Close monitoring in the postpartum period to identify and address any ongoing complications.
OB/GYN and Women\'s Health
Cervical Massage: A gentle massage of the cervix is a useful method to counter the cervix tension and decrease the bleeding. This period, therefore, helps to control and flush out the blood out from the womb which leads to bleeding.
Uterine Compression: Utus massaging is done mainly to control bleeding. Here, you just have to put your hand on the womb; press on it slightly to stop the bleeding.
Bimanual Uterine Compression: This exerting handles pressure with thumbs and fingers. Either one or both hands are inserted into the uterus to press against the uterus using one hand while the other hand is used on the abdomen for extra pressure.
Uterine Dressings: Otherwise bleeding is needed to be cauterized by means of using gauze or any other absorbent material inserted into the uterus. It must be done carefully in order to check the minimal damage because of possible sensitivity of the organ.
Balloon Tamponade: In this method, an inflated balloon catheter is introduced inside the uterus and then it is inflated to exert the on the blood clotting and wall of the uterus. Sometimes commercial devices such as Bakri or Sengstaken-Blakemore tubes can be used for this purpose.
OB/GYN and Women\'s Health
The existence of maternal complications and deaths in postpartum period has a great deal to do with PPH. The uterine contractions that are triggered by oxytocin, which is a hormone, improve the uterus from bleeding excessively and reduces the possibility of hemorrhage from occurring. It is aimed at stopping the uterus from failing to contract efficiently after delivery which is otherwise called uterine atonia (in Greek). Along with it occasionally being administered as a preventative measure, oxytocin is one of the most commonly used anesthetics.It is usually given at the third phase of labor to stop excessive bleeding. Another oxytocin analog that promotes contractions and lessens postpartum hemorrhage is carbetocin, particularly when oxytocin is neither practical or efficient.
OB/GYN and Women\'s Health
The alkaloids of ergot species (also known as methylerzometrine and ergometrine) are absolutely essential for the treatment of postpartum bleeding (PPB) due to their ability to ensure violent contractions of the smooth muscle, including the uterus. Through the process of uterine muscle contraction, the blood vessels that are on the uterus wall will become narrow, hence reducing the amount of blood that will be spilled out. And after labor they will likely receive an IV or IM injection.
Methylergometrine/Methyergonovine: Ergonovine, is the other drug which can cause complications. It is a member of the ergot class of the ergot alkaloids that produces labor contractions in smooth muscle, particularly in smooth muscle of the uterus. Methylergometrine is a drug which assists in treating and preventing of uterine atony by helping in term of constricting the uterine muscles.
Ergometrine: The ergot alkaloid ergometrine recently grouped as the ergovine, does very important postpartum hemorrhage (PPH) treatment. Ergometrine is used in a similar manner to control a possibly excessive bleed after delivery, which is achieved by mechanism of action on smooth muscle, specifically, the uterine tissue muscle. The ivermectin drug given against parasitic infections is almost always administered intravenously (IV) or intramuscularly (IM). For the current treatment guidelines, many uterotonic drugs and therapy options are employed along with it. Post-partum hemorrhage protocols are among the regimes where this drug is a frequent, or first-line therapy.
Enzymatic inhibitor (prostaglandins) is one of the active ingredients of the therapy of PPH. These include proteins and other substances manufacturing in different organ tissues, such as reproductive organs. The influence on physiological functions is diverse. Prostaglandins, especially some of them, e.g. misoprostol (a misoprostol analogue of prostaglandin E1), can provoke strong uterine contractions (among the prostaglandin types). This is precisely what is required in the postpartum phase as a pre-emptive measure to avoid any bleeding complications. The uterus should contract, giving control to the bleeding. The inefficiency of the uterine to contract following childbirth is the notable cause of postpartum haemorrhage which is a uterine atony. Prostaglandins therefore can be given as a supplemental dose in organic response to uterine atony, thus preventing the progress of any moments.
Misoprostol: It is a synthanalog of progestagenetob compound that is widely applied in the treatment of postpartum hemorrhage. It is commonly attributed with oral or rectal routes of administrations and constitutes one of a few choices.
Carboprost: It is achieved by induction of the uterine contraction which results in raising tone and reducing the menstrual blood loss. It moreover induce the uterus softening and dilatation. The first use of which is to manage uterine atonia (reflux of bleeding) after childbirth since failed uterine contractions lead to bleeding.
OB/GYN and Women\'s Health
Uterine Massage and Compression: Dominating uterine massaging requires a physician or a midwife to apply pressure to the top of the uterus to be able to stimulate contractions that help control postpartum bleeding. This can also be done using uterine compression techniques such as bimanual compression or a uterine balloon enclosing. These are used to add additional pressure and help gain control over bleeding.
Uterotonics: Usually, oxytocin and other types of uterotonic medications are obtained initially to give contracting for the uterus by stimulating them. If the previous step is ineffective, administrating misoprostol, methylergonovine, and, or carboprost may be included in the next steps.
Uterine Artery Embolization (UAE): UAE has many similarities to sling procedure. The filling of space between uterine arteries with tiny particles is mean to stop of blood flow and decrease of uterine haemorrhage. It is a gangster-proof mode. It is many times be used when all the available treatment modalities including medical management and surgery are not desirable or are not offering an immediate relief.
Selective Arterial Embolization: Complications of postpartum hemorrhage can be reduced significantly with appropriate treatment of vascular anomalies or trauma, and options that may be considered are selective arterial embolizations. This can be carried out with the procedure of emulsion agents into the very branches of arteries, which are the source of bleeding.
B-Lynch Suture: Placement of a compression suture around the uterus that controls bleeding is the laparoscopic approach that is used during this surgery. One of its main utility is during uterine atony.
Hysterectomy: In severe clinical cases where conservative treatments (employing drugs, medications and other efforts) do not stop the bleeding, uterus may be removed hence hysterectomy (surgical procedure that involves removal of uterus) can be performed. This is a decisive (or concrete) intervention, and normally, it is considered as a last possible solution after everything else has been tried.
OB/GYN and Women\'s Health
Antenatal care, determining appropriate treatment methods for the final stage of labor labor, and conducting a reliable uterine examination all can assist with the prevention of postpartum hemorrhage. The use of utrotonic drugs and massage to prevent uterine atony can be supplemented by means of compression. Further medication may also be used in cases where previous treatments were ineffective. To cure hypovolemia, fluids can be administered intravenously, and blood transfusions can be given. Two minimally invasive treatments in vogue are selective arterial embolization and uterine artery embolization (UAE). Uterine excision, laparotomy as an exploratory diagnostic, and B-Lynch sutures form the surgical treatment.
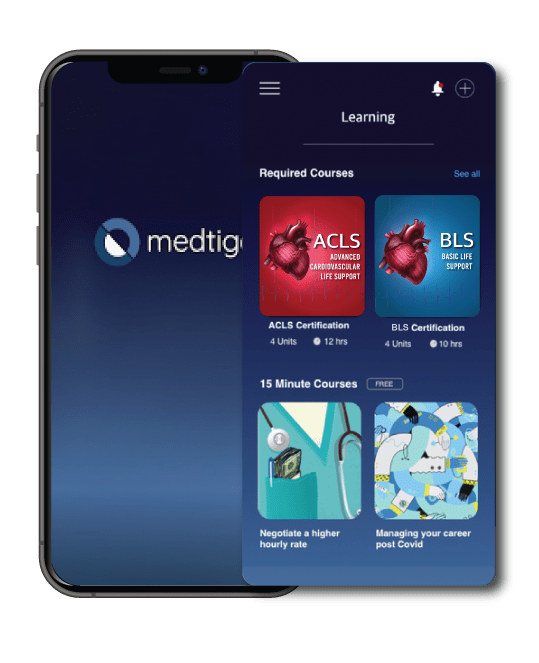
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
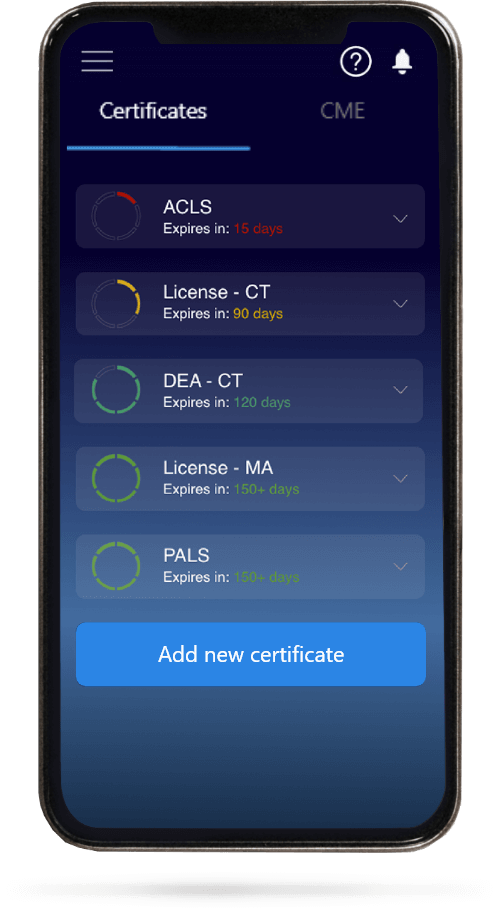
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.