Can Extra Weekend Sleep Improve Glucose Health? What Researchers Found
March 4, 2026
Background
Primary biliary cholangitis, which was previously called primary biliary cirrhosis, is an autoimmune disorder that develops slowly. Over time, the intrahepatic bile ducts get destroyed and hence the result is periportal inflammation and cirrhosis. Prolonged hepatic cholestasis causes liver to be replaced by fibrous tissue and this also contributes to the elevation of blood pressure in the blood vessels that bring blood from intestines to liver which is known as portal hypertension. The principal cholestatic disease of middle-aged women in the United States is primary cholangitis.
Epidemiology
The true incidence of primary biliary cholangitis is continuously increasing due to the more the screening tests that are performed, like liver chemistry and lipid profile that are used to rule out other issues utilized in otherwise young/healthy individuals. The world suffers from primary biliary cholangitis with middle-aged women being affected largely. The females to males ratio is 9:1. The usual form of this disease happens in women during the age of 30 and 60. Primary biliary cholangitis is a liver disease primarily found in Europe and North America. But the age-tested data in the different countries shows a large number of cases. The incidence of primary biliary cirrhosis standardized by population was 45 per 1 million person-years for women and was 7 per 1 million person-years for men in the United States, while the prevalence was 654 per 1 million persons in women and 121 in men.
Anatomy
Pathophysiology
Both the genetic predisposition and environment have effects on the development of PBC. It is quite common to first-degree relatives, and it means that more often a case occurs in monozygotic twins. Girls of affected women who are more than twenty-four years old are at most risk. HLA alleles including, DRB1, DR3, DPB1, DQA1, and DQB1, have been connected to Primary Biliary Cirrhosis, and HLA-DRB1*08 is common in European and Asian nature and HLA-DRB1*11 has the shield effect.
Other environmental causes that are responsible for it are heavy metal polluted waste, cigarette smoking, nail polish, hair dye, and xenobiotics like Escherichia coli, Mycobacterium gordonae, and Novosphingobium aromaticivorans. These triggers are able with the help of the immune gram to induce an autoimmune reaction in genetically susceptible individuals. This leads to the humoral and cellular response to an antigen, specific anti-mitochondrial antibodies, and T lymphocyte involvement in bile duct destruction are then formed. Bacteria with lipoylated proteins can also trigger an immune response.
This is also linked to specific autoantibodies, as the antimitochondrial antibody (AMA) is present in 85% of cases and is the most responsible, in this case, for the primary target of mitochondria. Other types of antibodies that are very strongly connected to PBC include ANA, AMND, ACEN, and ANEA. The following two antibodies are particularly informative for AMA negative PBC: ANA and AMND.
Etiology
Primary biliary cholangitis (PBC) represents an autoimmune disease. Experts speculate that principle biliary cirrhosis patients are both genetically predisposed and exposed to the environmental trigger. First-degree relatives of the index patient suffer from the disease at a rate one hundred times greater than the general population, providing strong evidence of a genetic predisposition. The investigations have led to the conclusion that environmental triggers play a significant role as is depicted by the presence of urinary tract infection, reproductive hormone replacement, nail polish, cigarette smoking, and xenobiotics, among toxic waste sites. According to the research, the inflammation is considered here as a direct insult of environmental factors and toxins.
Genetics
Prognostic Factors
Primary biliary cholangitis can be diagnosed mainly by elevated serum bilirubin levels and the Mayo risk score. The outcome is linked to the bilirubin levels, and more bilirubin indicates more time left to live. Furthermore, the fatigue of the patient may be also evaluated as a prognostic indicator in this disease. Over 1.4 years, the survival of those who has that much consistency in the levels of bilirubin is above 10 mg/dL is the mean the highest.
Clinical History
Discomfort in right upper quadrant: Mostly 8-17% of people suffer from discomfort in the specified region.
Fatigue: It has become a common consequence of primary biliary cholangitis disease thus causing disability and depression. Although the cause is not known, sleep problems, especially excessive daytime somnolence, are most frequent. There does not exist a direct relationship between tiredness and liver disease stage, enzyme levels, Mayo model score, or therapy duration. The nature of fatigue is vague, but based on some data, the hypothalamic-pituitary-adrenal axis disorders, like reduced serotonin release, and the enhanced formation of proinflammatory cytokines, are potential possibilities. However, the question for fatigue is unclear because there is some evidence for a link with hypothalamic-pituitary-adrenal axis abnormalities, such as decreased serotonin release production and increased proinflammatory cytokine production.
Pruritis: Around 10% of people with primary biliary cholangitis, suffer from high level itching which is so grave at night, during hot weather as well as when their body skins are dry.
Physical Examination
Physical tests to check for the existence of the disease depends on the stage that the disease is in. In the initial stage, there are usually no abnormalities. But as disease advacnes, patients show marks of skin excoriations, xanthomas, xanthelasmas, or cirrhosis signs.
Additional findings that can be considered include:
Age group
Associated comorbidity
Bone disease
Fat-soluble vitamin deficiency
Hyperlipidemia
Pruritis
Steatorrhea
Liver transplant
Associated activity
Acuity of presentation
Differential Diagnoses
Biliary obstruction
Autoimmune hepatitis
Drug-induced hepatotoxicity
Primary Sclerosing cholangitis
Graft-versus host disease
Sarcoidosis
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
Ursodeoxycholic acid: PBC is primarily treated by using UDCA as an initial therapy because it helps enhance liver operationality and check the disease from spreading through steps that include improving the excretion of bile while at the same time reducing its toxicity.
Obeticholic acid: If UDCA is not enough or cannot be tolerated by the patient, the prescription of OCA might be considered. OCA is an agonist of farnesoid X receptor, which may lead to an improvement in liver function test results and possibly delay progression of illness.
Symptomatic management: Itching associated with pbc can be alleviated with antihistamines as well as cholestyramine or rifampin, while for the malabsorption of vitamins mineral oils chelates must be included in it too.
Liver transplant: When someone has terminal liver cirrhosis or liver failure, they might want to consider having a liver transplant.
Monitoring and supportive care: The care of patients with PBC involves in the liver function tests, imaging studies monitoring as well as symptom management that means these aspects are necessary to guarantee.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
modification-of-environment
Avoidance of toxins and xenobiotics:
Patients that have primary cirrhosis of the liver (PBC) want to limit their contact with environmental pollutants that are poisonous like cigarette smoke as well as harmful substances polluting the air that can aggravate the state of liver function leading to inflammation of this organ.
Healthy lifestyle choices:
In order to maintain good liver health, it is essential to encourage a healthy diet that is high in fruits, vegetables and whole grains. Additionally excessive consumption of alcohol must be avoided which may harm the liver.
Managing stress:
About minimizing stress levels, stress reduction techniques such as meditation and counselling among others are very important because they help in promoting a positive effect on the health.
Use of bile acids
Ursodiol: This displaces the endogenous bile acids from enterohepatic circulation, stabilizes hepatocellular membranes and reduces the abnormal expression of class I and II molecules on hepatocytes.
Use of Farnesoid X receptor agonist
Obeticholic acid: This drug is an agonist of FXR (farnesoid X receptor). Activation of FXR inhibits the de novo synthesis of bile acids along with an increase in the transportation of bile acids from the hepatocytes which reduces the exposure of hepatocytes to bile acids. It is primarily indicated in treating primary biliary cholangitis along with UDCA (ursodeoxycholic acid).
Use of PPAR (peroxisome proliferator- activated receptor) agonists
PPAR agonists are believed to cause a FGF21 (fibroblast growth factor)-dependent reduction in CYP7A1, the main enzyme responsible for converting cholesterol into bile acids.
Elafibranor: This medicine is indicated in treating PBC along with UDCA in adults who had unsatisfactory response to UDCA or in cases where patients could not tolerate UDCA monotherapy.
Use of immunosuppressants
Methotrexate: An improvement in histologic and biochemical results is observed in various clinical trials after using this drug.
Prednisolone: This is known to improve symptoms, histologic and biochemical findings.
Use of anti-inflammatory agents
Colchicine: This has been administered to patients, but the results were controversial. This class of drugs are used to reduce the motility of leukocytes and phagocytosis in inflammation.
Use of antipruritic agents
Cholestyramine: It effectively sequesters the bile salts in the lumen of intestine, but typically takes one to four days for itching to subside.
Rifampin: The exact mechanism of action is unknown. This may include inhibition of uptake of bile acids into hepatocytes.
Colestipol: This is known to form a soluble complex after binding to bile acids thereby increasing the loss of bile acids through feces.
Use of antihistamines
Hydroxyzine hydrochloride: This antagonizes the H1 receptors in the periphery and it might suppress the activity of histamines in the subcortical region of central nervous system.
intervention-with-a-procedure
Liver transplantation: Upregulated bilirubin levels, lengthened prothrombin time, and reduced albumin levels are signs of cirrhosis, which necessitates liver transplantation. An overall survival rate of 80% has been achieved at five years with this procedure which is the only life-saving technique.
use-of-phases-of-management-in-treating-primary-biliary-cholangitis
Due to the fact that its morbidity and mortality rates are high, primary biliary cholangitis (PBC) calls for a multidisciplinary approach team. The goal of the treatment is to slow down the progression of the disease and improve the quality of life. In patient care, special attention is paid to the role of nurses, nurses, mental health counsellors, pharmacists, and physical therapists. Patients should be tught about management of itching, diet, Sicca syndrome, and regular physical exercises.
Medication
Initially, 5 mg orally each day
Maintenance dose- 5 mg orally each day
If no reduction is seen in alkaline phosphatase or total bilirubin after 3 months, increase the dose to 10 mg orally each day
Maximum dose-10 mg each day
The recommended daily dose based on body weight is 10mg/kg
12 to 15mg/kg/day, equivalent to 600 to 1000mg orally once a day in two to three divided doses
Future Trends
Primary biliary cholangitis, which was previously called primary biliary cirrhosis, is an autoimmune disorder that develops slowly. Over time, the intrahepatic bile ducts get destroyed and hence the result is periportal inflammation and cirrhosis. Prolonged hepatic cholestasis causes liver to be replaced by fibrous tissue and this also contributes to the elevation of blood pressure in the blood vessels that bring blood from intestines to liver which is known as portal hypertension. The principal cholestatic disease of middle-aged women in the United States is primary cholangitis.
The true incidence of primary biliary cholangitis is continuously increasing due to the more the screening tests that are performed, like liver chemistry and lipid profile that are used to rule out other issues utilized in otherwise young/healthy individuals. The world suffers from primary biliary cholangitis with middle-aged women being affected largely. The females to males ratio is 9:1. The usual form of this disease happens in women during the age of 30 and 60. Primary biliary cholangitis is a liver disease primarily found in Europe and North America. But the age-tested data in the different countries shows a large number of cases. The incidence of primary biliary cirrhosis standardized by population was 45 per 1 million person-years for women and was 7 per 1 million person-years for men in the United States, while the prevalence was 654 per 1 million persons in women and 121 in men.
Both the genetic predisposition and environment have effects on the development of PBC. It is quite common to first-degree relatives, and it means that more often a case occurs in monozygotic twins. Girls of affected women who are more than twenty-four years old are at most risk. HLA alleles including, DRB1, DR3, DPB1, DQA1, and DQB1, have been connected to Primary Biliary Cirrhosis, and HLA-DRB1*08 is common in European and Asian nature and HLA-DRB1*11 has the shield effect.
Other environmental causes that are responsible for it are heavy metal polluted waste, cigarette smoking, nail polish, hair dye, and xenobiotics like Escherichia coli, Mycobacterium gordonae, and Novosphingobium aromaticivorans. These triggers are able with the help of the immune gram to induce an autoimmune reaction in genetically susceptible individuals. This leads to the humoral and cellular response to an antigen, specific anti-mitochondrial antibodies, and T lymphocyte involvement in bile duct destruction are then formed. Bacteria with lipoylated proteins can also trigger an immune response.
This is also linked to specific autoantibodies, as the antimitochondrial antibody (AMA) is present in 85% of cases and is the most responsible, in this case, for the primary target of mitochondria. Other types of antibodies that are very strongly connected to PBC include ANA, AMND, ACEN, and ANEA. The following two antibodies are particularly informative for AMA negative PBC: ANA and AMND.
Primary biliary cholangitis (PBC) represents an autoimmune disease. Experts speculate that principle biliary cirrhosis patients are both genetically predisposed and exposed to the environmental trigger. First-degree relatives of the index patient suffer from the disease at a rate one hundred times greater than the general population, providing strong evidence of a genetic predisposition. The investigations have led to the conclusion that environmental triggers play a significant role as is depicted by the presence of urinary tract infection, reproductive hormone replacement, nail polish, cigarette smoking, and xenobiotics, among toxic waste sites. According to the research, the inflammation is considered here as a direct insult of environmental factors and toxins.
Primary biliary cholangitis can be diagnosed mainly by elevated serum bilirubin levels and the Mayo risk score. The outcome is linked to the bilirubin levels, and more bilirubin indicates more time left to live. Furthermore, the fatigue of the patient may be also evaluated as a prognostic indicator in this disease. Over 1.4 years, the survival of those who has that much consistency in the levels of bilirubin is above 10 mg/dL is the mean the highest.
Discomfort in right upper quadrant: Mostly 8-17% of people suffer from discomfort in the specified region.
Fatigue: It has become a common consequence of primary biliary cholangitis disease thus causing disability and depression. Although the cause is not known, sleep problems, especially excessive daytime somnolence, are most frequent. There does not exist a direct relationship between tiredness and liver disease stage, enzyme levels, Mayo model score, or therapy duration. The nature of fatigue is vague, but based on some data, the hypothalamic-pituitary-adrenal axis disorders, like reduced serotonin release, and the enhanced formation of proinflammatory cytokines, are potential possibilities. However, the question for fatigue is unclear because there is some evidence for a link with hypothalamic-pituitary-adrenal axis abnormalities, such as decreased serotonin release production and increased proinflammatory cytokine production.
Pruritis: Around 10% of people with primary biliary cholangitis, suffer from high level itching which is so grave at night, during hot weather as well as when their body skins are dry.
Physical tests to check for the existence of the disease depends on the stage that the disease is in. In the initial stage, there are usually no abnormalities. But as disease advacnes, patients show marks of skin excoriations, xanthomas, xanthelasmas, or cirrhosis signs.
Additional findings that can be considered include:
Bone disease
Fat-soluble vitamin deficiency
Hyperlipidemia
Pruritis
Steatorrhea
Liver transplant
Biliary obstruction
Autoimmune hepatitis
Drug-induced hepatotoxicity
Primary Sclerosing cholangitis
Graft-versus host disease
Sarcoidosis
Ursodeoxycholic acid: PBC is primarily treated by using UDCA as an initial therapy because it helps enhance liver operationality and check the disease from spreading through steps that include improving the excretion of bile while at the same time reducing its toxicity.
Obeticholic acid: If UDCA is not enough or cannot be tolerated by the patient, the prescription of OCA might be considered. OCA is an agonist of farnesoid X receptor, which may lead to an improvement in liver function test results and possibly delay progression of illness.
Symptomatic management: Itching associated with pbc can be alleviated with antihistamines as well as cholestyramine or rifampin, while for the malabsorption of vitamins mineral oils chelates must be included in it too.
Liver transplant: When someone has terminal liver cirrhosis or liver failure, they might want to consider having a liver transplant.
Monitoring and supportive care: The care of patients with PBC involves in the liver function tests, imaging studies monitoring as well as symptom management that means these aspects are necessary to guarantee.
Gastroenterology
Avoidance of toxins and xenobiotics:
Patients that have primary cirrhosis of the liver (PBC) want to limit their contact with environmental pollutants that are poisonous like cigarette smoke as well as harmful substances polluting the air that can aggravate the state of liver function leading to inflammation of this organ.
Healthy lifestyle choices:
In order to maintain good liver health, it is essential to encourage a healthy diet that is high in fruits, vegetables and whole grains. Additionally excessive consumption of alcohol must be avoided which may harm the liver.
Managing stress:
About minimizing stress levels, stress reduction techniques such as meditation and counselling among others are very important because they help in promoting a positive effect on the health.
Gastroenterology
Ursodiol: This displaces the endogenous bile acids from enterohepatic circulation, stabilizes hepatocellular membranes and reduces the abnormal expression of class I and II molecules on hepatocytes.
Gastroenterology
Obeticholic acid: This drug is an agonist of FXR (farnesoid X receptor). Activation of FXR inhibits the de novo synthesis of bile acids along with an increase in the transportation of bile acids from the hepatocytes which reduces the exposure of hepatocytes to bile acids. It is primarily indicated in treating primary biliary cholangitis along with UDCA (ursodeoxycholic acid).
Gastroenterology
PPAR agonists are believed to cause a FGF21 (fibroblast growth factor)-dependent reduction in CYP7A1, the main enzyme responsible for converting cholesterol into bile acids.
Elafibranor: This medicine is indicated in treating PBC along with UDCA in adults who had unsatisfactory response to UDCA or in cases where patients could not tolerate UDCA monotherapy.
Gastroenterology
Methotrexate: An improvement in histologic and biochemical results is observed in various clinical trials after using this drug.
Prednisolone: This is known to improve symptoms, histologic and biochemical findings.
Gastroenterology
Colchicine: This has been administered to patients, but the results were controversial. This class of drugs are used to reduce the motility of leukocytes and phagocytosis in inflammation.
Gastroenterology
Cholestyramine: It effectively sequesters the bile salts in the lumen of intestine, but typically takes one to four days for itching to subside.
Rifampin: The exact mechanism of action is unknown. This may include inhibition of uptake of bile acids into hepatocytes.
Colestipol: This is known to form a soluble complex after binding to bile acids thereby increasing the loss of bile acids through feces.
Gastroenterology
Hydroxyzine hydrochloride: This antagonizes the H1 receptors in the periphery and it might suppress the activity of histamines in the subcortical region of central nervous system.
Gastroenterology
Liver transplantation: Upregulated bilirubin levels, lengthened prothrombin time, and reduced albumin levels are signs of cirrhosis, which necessitates liver transplantation. An overall survival rate of 80% has been achieved at five years with this procedure which is the only life-saving technique.
Gastroenterology
Due to the fact that its morbidity and mortality rates are high, primary biliary cholangitis (PBC) calls for a multidisciplinary approach team. The goal of the treatment is to slow down the progression of the disease and improve the quality of life. In patient care, special attention is paid to the role of nurses, nurses, mental health counsellors, pharmacists, and physical therapists. Patients should be tught about management of itching, diet, Sicca syndrome, and regular physical exercises.
Primary biliary cholangitis, which was previously called primary biliary cirrhosis, is an autoimmune disorder that develops slowly. Over time, the intrahepatic bile ducts get destroyed and hence the result is periportal inflammation and cirrhosis. Prolonged hepatic cholestasis causes liver to be replaced by fibrous tissue and this also contributes to the elevation of blood pressure in the blood vessels that bring blood from intestines to liver which is known as portal hypertension. The principal cholestatic disease of middle-aged women in the United States is primary cholangitis.
The true incidence of primary biliary cholangitis is continuously increasing due to the more the screening tests that are performed, like liver chemistry and lipid profile that are used to rule out other issues utilized in otherwise young/healthy individuals. The world suffers from primary biliary cholangitis with middle-aged women being affected largely. The females to males ratio is 9:1. The usual form of this disease happens in women during the age of 30 and 60. Primary biliary cholangitis is a liver disease primarily found in Europe and North America. But the age-tested data in the different countries shows a large number of cases. The incidence of primary biliary cirrhosis standardized by population was 45 per 1 million person-years for women and was 7 per 1 million person-years for men in the United States, while the prevalence was 654 per 1 million persons in women and 121 in men.
Both the genetic predisposition and environment have effects on the development of PBC. It is quite common to first-degree relatives, and it means that more often a case occurs in monozygotic twins. Girls of affected women who are more than twenty-four years old are at most risk. HLA alleles including, DRB1, DR3, DPB1, DQA1, and DQB1, have been connected to Primary Biliary Cirrhosis, and HLA-DRB1*08 is common in European and Asian nature and HLA-DRB1*11 has the shield effect.
Other environmental causes that are responsible for it are heavy metal polluted waste, cigarette smoking, nail polish, hair dye, and xenobiotics like Escherichia coli, Mycobacterium gordonae, and Novosphingobium aromaticivorans. These triggers are able with the help of the immune gram to induce an autoimmune reaction in genetically susceptible individuals. This leads to the humoral and cellular response to an antigen, specific anti-mitochondrial antibodies, and T lymphocyte involvement in bile duct destruction are then formed. Bacteria with lipoylated proteins can also trigger an immune response.
This is also linked to specific autoantibodies, as the antimitochondrial antibody (AMA) is present in 85% of cases and is the most responsible, in this case, for the primary target of mitochondria. Other types of antibodies that are very strongly connected to PBC include ANA, AMND, ACEN, and ANEA. The following two antibodies are particularly informative for AMA negative PBC: ANA and AMND.
Primary biliary cholangitis (PBC) represents an autoimmune disease. Experts speculate that principle biliary cirrhosis patients are both genetically predisposed and exposed to the environmental trigger. First-degree relatives of the index patient suffer from the disease at a rate one hundred times greater than the general population, providing strong evidence of a genetic predisposition. The investigations have led to the conclusion that environmental triggers play a significant role as is depicted by the presence of urinary tract infection, reproductive hormone replacement, nail polish, cigarette smoking, and xenobiotics, among toxic waste sites. According to the research, the inflammation is considered here as a direct insult of environmental factors and toxins.
Primary biliary cholangitis can be diagnosed mainly by elevated serum bilirubin levels and the Mayo risk score. The outcome is linked to the bilirubin levels, and more bilirubin indicates more time left to live. Furthermore, the fatigue of the patient may be also evaluated as a prognostic indicator in this disease. Over 1.4 years, the survival of those who has that much consistency in the levels of bilirubin is above 10 mg/dL is the mean the highest.
Discomfort in right upper quadrant: Mostly 8-17% of people suffer from discomfort in the specified region.
Fatigue: It has become a common consequence of primary biliary cholangitis disease thus causing disability and depression. Although the cause is not known, sleep problems, especially excessive daytime somnolence, are most frequent. There does not exist a direct relationship between tiredness and liver disease stage, enzyme levels, Mayo model score, or therapy duration. The nature of fatigue is vague, but based on some data, the hypothalamic-pituitary-adrenal axis disorders, like reduced serotonin release, and the enhanced formation of proinflammatory cytokines, are potential possibilities. However, the question for fatigue is unclear because there is some evidence for a link with hypothalamic-pituitary-adrenal axis abnormalities, such as decreased serotonin release production and increased proinflammatory cytokine production.
Pruritis: Around 10% of people with primary biliary cholangitis, suffer from high level itching which is so grave at night, during hot weather as well as when their body skins are dry.
Physical tests to check for the existence of the disease depends on the stage that the disease is in. In the initial stage, there are usually no abnormalities. But as disease advacnes, patients show marks of skin excoriations, xanthomas, xanthelasmas, or cirrhosis signs.
Additional findings that can be considered include:
Bone disease
Fat-soluble vitamin deficiency
Hyperlipidemia
Pruritis
Steatorrhea
Liver transplant
Biliary obstruction
Autoimmune hepatitis
Drug-induced hepatotoxicity
Primary Sclerosing cholangitis
Graft-versus host disease
Sarcoidosis
Ursodeoxycholic acid: PBC is primarily treated by using UDCA as an initial therapy because it helps enhance liver operationality and check the disease from spreading through steps that include improving the excretion of bile while at the same time reducing its toxicity.
Obeticholic acid: If UDCA is not enough or cannot be tolerated by the patient, the prescription of OCA might be considered. OCA is an agonist of farnesoid X receptor, which may lead to an improvement in liver function test results and possibly delay progression of illness.
Symptomatic management: Itching associated with pbc can be alleviated with antihistamines as well as cholestyramine or rifampin, while for the malabsorption of vitamins mineral oils chelates must be included in it too.
Liver transplant: When someone has terminal liver cirrhosis or liver failure, they might want to consider having a liver transplant.
Monitoring and supportive care: The care of patients with PBC involves in the liver function tests, imaging studies monitoring as well as symptom management that means these aspects are necessary to guarantee.
Gastroenterology
Avoidance of toxins and xenobiotics:
Patients that have primary cirrhosis of the liver (PBC) want to limit their contact with environmental pollutants that are poisonous like cigarette smoke as well as harmful substances polluting the air that can aggravate the state of liver function leading to inflammation of this organ.
Healthy lifestyle choices:
In order to maintain good liver health, it is essential to encourage a healthy diet that is high in fruits, vegetables and whole grains. Additionally excessive consumption of alcohol must be avoided which may harm the liver.
Managing stress:
About minimizing stress levels, stress reduction techniques such as meditation and counselling among others are very important because they help in promoting a positive effect on the health.
Gastroenterology
Ursodiol: This displaces the endogenous bile acids from enterohepatic circulation, stabilizes hepatocellular membranes and reduces the abnormal expression of class I and II molecules on hepatocytes.
Gastroenterology
Obeticholic acid: This drug is an agonist of FXR (farnesoid X receptor). Activation of FXR inhibits the de novo synthesis of bile acids along with an increase in the transportation of bile acids from the hepatocytes which reduces the exposure of hepatocytes to bile acids. It is primarily indicated in treating primary biliary cholangitis along with UDCA (ursodeoxycholic acid).
Gastroenterology
PPAR agonists are believed to cause a FGF21 (fibroblast growth factor)-dependent reduction in CYP7A1, the main enzyme responsible for converting cholesterol into bile acids.
Elafibranor: This medicine is indicated in treating PBC along with UDCA in adults who had unsatisfactory response to UDCA or in cases where patients could not tolerate UDCA monotherapy.
Gastroenterology
Methotrexate: An improvement in histologic and biochemical results is observed in various clinical trials after using this drug.
Prednisolone: This is known to improve symptoms, histologic and biochemical findings.
Gastroenterology
Colchicine: This has been administered to patients, but the results were controversial. This class of drugs are used to reduce the motility of leukocytes and phagocytosis in inflammation.
Gastroenterology
Cholestyramine: It effectively sequesters the bile salts in the lumen of intestine, but typically takes one to four days for itching to subside.
Rifampin: The exact mechanism of action is unknown. This may include inhibition of uptake of bile acids into hepatocytes.
Colestipol: This is known to form a soluble complex after binding to bile acids thereby increasing the loss of bile acids through feces.
Gastroenterology
Hydroxyzine hydrochloride: This antagonizes the H1 receptors in the periphery and it might suppress the activity of histamines in the subcortical region of central nervous system.
Gastroenterology
Liver transplantation: Upregulated bilirubin levels, lengthened prothrombin time, and reduced albumin levels are signs of cirrhosis, which necessitates liver transplantation. An overall survival rate of 80% has been achieved at five years with this procedure which is the only life-saving technique.
Gastroenterology
Due to the fact that its morbidity and mortality rates are high, primary biliary cholangitis (PBC) calls for a multidisciplinary approach team. The goal of the treatment is to slow down the progression of the disease and improve the quality of life. In patient care, special attention is paid to the role of nurses, nurses, mental health counsellors, pharmacists, and physical therapists. Patients should be tught about management of itching, diet, Sicca syndrome, and regular physical exercises.
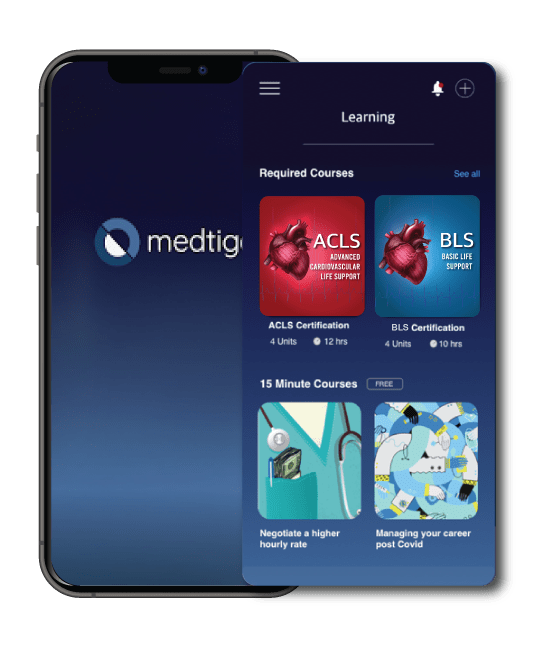
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
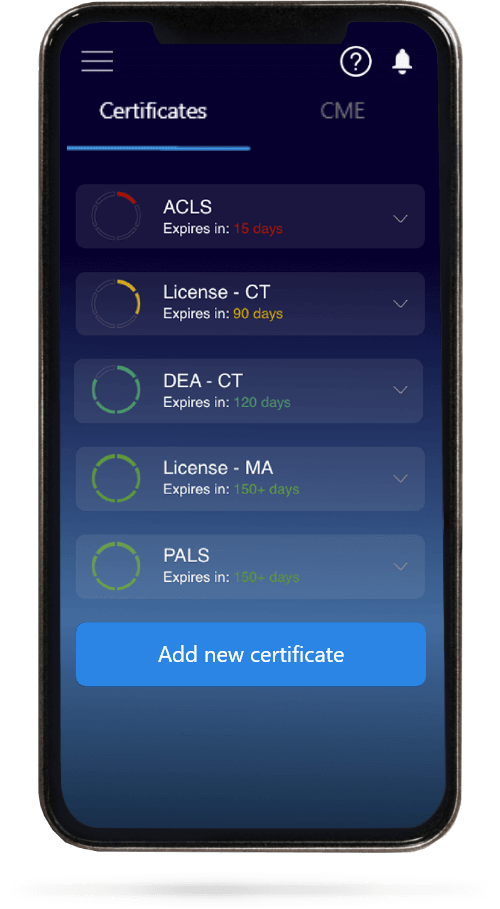
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.