Ostarine: The ‘Invisible’ Doping Threat Trapping Innocent Athletes
February 18, 2026
Background
Sickle cell anemia is a genetic blood disorder that typically affects people of Mediterranean, African, Middle Eastern, and Indian ancestry. This genetic disorder is caused by a mutation in the hemoglobin gene, which results in the production of aberrant hemoglobin known as hemoglobin S (HbS). This alteration of genetic mutation causes red blood cells to develop with a distinctive sickle shape, limited flexibility, and a proclivity to obstruct small blood veins.
Sickle cell anemia is the most common form of sickle cell disease (SCD), and it is distinguished by chronic hemolytic anemia that demands blood transfusions, periodic episodes of extreme pain, and persistent organ damage. Since the discovery of these unusual sickle-shaped red blood cells more than a century ago, our understanding of this illness has advanced tremendously.
Sickle cell anemia is an autosomal recessive genetic disorder, which means that both parents must carry the abnormal gene for a child to inherit the disease. If only one parent carries the gene, the child will be a carrier, but not necessarily affected by the disease. Hemoglobin is a protein in red blood cells responsible for carrying oxygen throughout the body. In individuals with sickle cell anemia, the presence of hemoglobin S causes red blood cells to take on a rigid, crescent or sickle shape when oxygen levels are low, such as during physical exertion or when oxygen demand is high. Over time, the repeated blockage of blood vessels can cause significant organ damage, including to the spleen, liver, lungs, and brain. People with sickle cell anemia are also at increased risk of stroke and various other health problems.
Epidemiology
There is a scarcity of epidemiological evidence regarding SCD. It is generally known that sub-Saharan Africa has higher rates of both SCD and HbAS, with HbAS carriers having a natural defense against severe Plasmodium falciparum malaria. Around 230,000 babies with SCA and over 3.5 million newborns with HbAS are thought to have been born in sub-Saharan Africa in 2010. Sub-Saharan Africa is thought to be the birthplace of 75% of babies with sickle cell disease. The majority of people with HbSC illness live in West Africa.
Roughly 100,000 Americans are thought to have sickle cell disease (SCD), according to the US Center for Disease Control (CDC). Additionally, according to the CDC, 1 in 365 African Americans and 1 in 13 newborns born to parents of African American descent have sickle cell disease (SCD). It is estimated that 1 in 16,300 Hispanic Americans have SCD. In the US, up to 40% of SCD patients are children and teenagers. States and the geographic areas where ethnic groups are concentrated affect the incidence. In addition, immigration from abroad and domestic mobility affect the prevalence of SCD and HbAS. This is accurate for patients with SCD and SCA residing in a number of nations.
Anatomy
Pathophysiology
Hemolysis and vaso-occlusive crisis (VOC) are the two primary characteristics of sickle cell anemia (SCA). Because of a beta-globin gene deficit, sickle hemoglobin (HbS) molecules are more likely to change into stiff, elongated polymers in a deoxygenated environment. At first, sickle erythrocytes go through a cyclical process in which they alternate between the normal biconcave shape and the abnormal crescent shape (which is developed at low oxygen pressure).
Deoxygenation encourages HbS polymerization and is caused by a number of sickle erythrocyte-specific variables, including poor oxygen affinity of HbS, physiologically elevated 2,3-diphosphoglycerate, and elevated sphingokinase-1 activity. The likelihood of HbS polymerization is further increased by excessive HbS concentrations, aberrant Gados channel activity that causes dehydration, and recurrent injury to the membrane of red blood cells (RBCs).
By causing HbS to autooxidize and causing damage to the erythrocyte cell membrane, oxidative stress plays a role in hemolysis. Within sickle RBCs, oxidative stress is elevated due to decreased expression of NADPH oxidase and increased expression of xanthine oxidase and dehydrogenase.
Etiology
Hemoglobin (Hb) is a significant protein found in red blood cells (RBCs). It consists of four globin chains, with two originating from alpha-globin (located on chromosome 16) and two from beta-globin (located on chromosome 11). There are various subtypes of Hb. The most common ones in adults who do not have hemoglobin disorders are as follows:
The sickle cell mutation arises when a negatively charged amino acid, glutamine, is replaced by a neutral amino acid, valine, at the sixth position of the beta-globin chain. This mutation follows Mendelian genetics and is inherited in an autosomal codominant manner. When someone has two copies of this mutation (homozygous), it results in the most severe form of sickle cell disease, known as SCA or HBSS disease. When beta-thalassemia and the sickle cell mutation are inherited together, it leads to HBS-Beta-0 disease, which has similar characteristics to HBSS disease.
On the other hand, inheriting one copy of the mutation (heterozygous) leads to the HbAS genotype. Individuals with HbAS are typically not considered to have the full spectrum of sickle cell disease, as many of them do not exhibit the usual symptoms of SCA. They may only be identified during events like childbirth, blood donation, or screening procedures.
Genetics
Prognostic Factors
Prognostic factors in sickle cell anemia (SCA) are elements or characteristics that can be utilized to anticipate how the disease will progress and what the outcome will be for individuals. These factors are valuable in gauging the seriousness of SCA and aiding in making treatment decisions. Key prognostic factors for sickle cell anemia encompass:
Clinical History
Physical Examination
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Differential Diagnoses
Sickle Cell Anemia (SCA) typically involves a combination of clinical assessment, laboratory tests, and genetic testing. However, there are other medical conditions and hemoglobinopathies that can present with similar symptoms or features, making it important to consider a differential diagnosis.
Other Hemoglobinopathies:
Hereditary Spherocytosis:
Hemolytic Anemias:
Iron-Deficiency Anemia:
Thalassemia Minor (Trait):
Other Hemoglobinopathies:
Infections:
Autoimmune Disorders:
Bone Marrow Disorders:
Hypoxia-Induced Symptoms:
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
The treatment paradigm for sickle cell anemia (SCA) encompasses addressing both immediate and long-term issues. Here is a concise overview of the key elements of this treatment plan:
Education and Genetic Counseling:
Complication Prevention:
Transplantation:
Supportive Care:
Psychosocial Support:
Managing Acute Complications:
Managing Chronic Pain:
Acute Chest Syndrome (ACS):
Sequestration Crises:
Acute Stroke:
Aplastic Crises:
Other Complications:
Chronic Complications:
Iron Overload:
Blood Transfusion:
This comprehensive treatment approach underscores the importance of personalized care and the collaboration of multiple healthcare specialties to ensure the best possible outcomes for individuals living with sickle cell anemia.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
Medication
Administer 1500mg orally every day
Hydroxyurea can be used along if needed
Dose Adjustments
Renal impairment: No dosage adjustment is necessary
Hepatic impairment:
Mild to moderate: No dosage adjustment necessary (Child A pugh or B)
Severe: Reduce to 1000 mg every day or 900 mg oral suspension orally every day (Child-Pugh C)
CYP3A4 inducers
Avoid administering CYP3A4 inducers in combination, whether they are strong or mild.
Increase dosage to 2500 mg orally once a day for strong CYP3A4 inducers.
Increase to 2,000 mg orally every day for moderate CYP3A4 inducers.
lovotibeglogene autotemcel (FDA Approval Pending)
FDA Approval Pending as one-time gene therapy for sickle cell disease in patients aged ≥12 years
According to response and blood count, the Initial dose of 15 mg/kg orally daily by 2.5 to 5 mg/kg every 12 weeks. Usual dosage: 15 to 30 mg/kg every day. Maximum dose: 35 mg/kg daily
Dose Adjustments
Dosing modifications
Renal impairment:
CrCl less than 60 ml/min: 7.5 mg/kg daily, titrate based on the response
Hepatic impairment: Severe (Child-Pugh score C): Contraindicated
It is an investigational drug studied for its effectiveness in the treatment of sickle cell disease
<30kg (<66 lb): Administer 5g orally twice a day
30 to 65 kgs (66 to 143 lb): Administer 10g orally twice a day
≥65kg (≥143 lb): Administer 15g orally twice a day
initial dose :
20
mg/kg
Orally
once a day
Increase 5 mg per kg per day every eight weeks depending on the severity <>br
maximum dose: 35 mg/kg per day
The blood counts need to be monitored
<4 years: Safety and efficacy not established
>12 years: Administer 1500mg orally every day
4 to 11 years:
10 to <20 kg: 600mg orally every day
20 to <40kg: 900mg orally every day
≥40kg: 1500mg orally every day
Dose Adjustments
Renal impairment: No dosage adjustment is necessary
Hepatic impairment:
Mild to moderate: No dosage adjustment necessary (Child A pugh or B)
Severe: Reduce to 1000 mg orally every day or 900 mg oral suspension orally every day (Child-Pugh C)
20 kg to <40kg: Reduce the dose to 600mg orally every day
10 kg to <20kg: Reduce the dosage to 300mg orally every day
lovotibeglogene autotemcel (FDA Approval Pending)
FDA Approval Pending as one-time gene therapy for sickle cell disease in patients aged ≥12 years
<5 years: Safety and efficacy not established
≥5 years: <30kg (<66 lb): Administer 5g orally twice a day
30 to 65 kgs (66 to 143 lb): Administer 10g orally twice a day
≥65kg (≥143 lb): Administer 15g orally twice a day
Future Trends
Sickle cell anemia is a genetic blood disorder that typically affects people of Mediterranean, African, Middle Eastern, and Indian ancestry. This genetic disorder is caused by a mutation in the hemoglobin gene, which results in the production of aberrant hemoglobin known as hemoglobin S (HbS). This alteration of genetic mutation causes red blood cells to develop with a distinctive sickle shape, limited flexibility, and a proclivity to obstruct small blood veins.
Sickle cell anemia is the most common form of sickle cell disease (SCD), and it is distinguished by chronic hemolytic anemia that demands blood transfusions, periodic episodes of extreme pain, and persistent organ damage. Since the discovery of these unusual sickle-shaped red blood cells more than a century ago, our understanding of this illness has advanced tremendously.
Sickle cell anemia is an autosomal recessive genetic disorder, which means that both parents must carry the abnormal gene for a child to inherit the disease. If only one parent carries the gene, the child will be a carrier, but not necessarily affected by the disease. Hemoglobin is a protein in red blood cells responsible for carrying oxygen throughout the body. In individuals with sickle cell anemia, the presence of hemoglobin S causes red blood cells to take on a rigid, crescent or sickle shape when oxygen levels are low, such as during physical exertion or when oxygen demand is high. Over time, the repeated blockage of blood vessels can cause significant organ damage, including to the spleen, liver, lungs, and brain. People with sickle cell anemia are also at increased risk of stroke and various other health problems.
There is a scarcity of epidemiological evidence regarding SCD. It is generally known that sub-Saharan Africa has higher rates of both SCD and HbAS, with HbAS carriers having a natural defense against severe Plasmodium falciparum malaria. Around 230,000 babies with SCA and over 3.5 million newborns with HbAS are thought to have been born in sub-Saharan Africa in 2010. Sub-Saharan Africa is thought to be the birthplace of 75% of babies with sickle cell disease. The majority of people with HbSC illness live in West Africa.
Roughly 100,000 Americans are thought to have sickle cell disease (SCD), according to the US Center for Disease Control (CDC). Additionally, according to the CDC, 1 in 365 African Americans and 1 in 13 newborns born to parents of African American descent have sickle cell disease (SCD). It is estimated that 1 in 16,300 Hispanic Americans have SCD. In the US, up to 40% of SCD patients are children and teenagers. States and the geographic areas where ethnic groups are concentrated affect the incidence. In addition, immigration from abroad and domestic mobility affect the prevalence of SCD and HbAS. This is accurate for patients with SCD and SCA residing in a number of nations.
Hemolysis and vaso-occlusive crisis (VOC) are the two primary characteristics of sickle cell anemia (SCA). Because of a beta-globin gene deficit, sickle hemoglobin (HbS) molecules are more likely to change into stiff, elongated polymers in a deoxygenated environment. At first, sickle erythrocytes go through a cyclical process in which they alternate between the normal biconcave shape and the abnormal crescent shape (which is developed at low oxygen pressure).
Deoxygenation encourages HbS polymerization and is caused by a number of sickle erythrocyte-specific variables, including poor oxygen affinity of HbS, physiologically elevated 2,3-diphosphoglycerate, and elevated sphingokinase-1 activity. The likelihood of HbS polymerization is further increased by excessive HbS concentrations, aberrant Gados channel activity that causes dehydration, and recurrent injury to the membrane of red blood cells (RBCs).
By causing HbS to autooxidize and causing damage to the erythrocyte cell membrane, oxidative stress plays a role in hemolysis. Within sickle RBCs, oxidative stress is elevated due to decreased expression of NADPH oxidase and increased expression of xanthine oxidase and dehydrogenase.
Hemoglobin (Hb) is a significant protein found in red blood cells (RBCs). It consists of four globin chains, with two originating from alpha-globin (located on chromosome 16) and two from beta-globin (located on chromosome 11). There are various subtypes of Hb. The most common ones in adults who do not have hemoglobin disorders are as follows:
The sickle cell mutation arises when a negatively charged amino acid, glutamine, is replaced by a neutral amino acid, valine, at the sixth position of the beta-globin chain. This mutation follows Mendelian genetics and is inherited in an autosomal codominant manner. When someone has two copies of this mutation (homozygous), it results in the most severe form of sickle cell disease, known as SCA or HBSS disease. When beta-thalassemia and the sickle cell mutation are inherited together, it leads to HBS-Beta-0 disease, which has similar characteristics to HBSS disease.
On the other hand, inheriting one copy of the mutation (heterozygous) leads to the HbAS genotype. Individuals with HbAS are typically not considered to have the full spectrum of sickle cell disease, as many of them do not exhibit the usual symptoms of SCA. They may only be identified during events like childbirth, blood donation, or screening procedures.
Prognostic factors in sickle cell anemia (SCA) are elements or characteristics that can be utilized to anticipate how the disease will progress and what the outcome will be for individuals. These factors are valuable in gauging the seriousness of SCA and aiding in making treatment decisions. Key prognostic factors for sickle cell anemia encompass:
Sickle Cell Anemia (SCA) typically involves a combination of clinical assessment, laboratory tests, and genetic testing. However, there are other medical conditions and hemoglobinopathies that can present with similar symptoms or features, making it important to consider a differential diagnosis.
Other Hemoglobinopathies:
Hereditary Spherocytosis:
Hemolytic Anemias:
Iron-Deficiency Anemia:
Thalassemia Minor (Trait):
Other Hemoglobinopathies:
Infections:
Autoimmune Disorders:
Bone Marrow Disorders:
Hypoxia-Induced Symptoms:
The treatment paradigm for sickle cell anemia (SCA) encompasses addressing both immediate and long-term issues. Here is a concise overview of the key elements of this treatment plan:
Education and Genetic Counseling:
Complication Prevention:
Transplantation:
Supportive Care:
Psychosocial Support:
Managing Acute Complications:
Managing Chronic Pain:
Acute Chest Syndrome (ACS):
Sequestration Crises:
Acute Stroke:
Aplastic Crises:
Other Complications:
Chronic Complications:
Iron Overload:
Blood Transfusion:
This comprehensive treatment approach underscores the importance of personalized care and the collaboration of multiple healthcare specialties to ensure the best possible outcomes for individuals living with sickle cell anemia.
Sickle cell anemia is a genetic blood disorder that typically affects people of Mediterranean, African, Middle Eastern, and Indian ancestry. This genetic disorder is caused by a mutation in the hemoglobin gene, which results in the production of aberrant hemoglobin known as hemoglobin S (HbS). This alteration of genetic mutation causes red blood cells to develop with a distinctive sickle shape, limited flexibility, and a proclivity to obstruct small blood veins.
Sickle cell anemia is the most common form of sickle cell disease (SCD), and it is distinguished by chronic hemolytic anemia that demands blood transfusions, periodic episodes of extreme pain, and persistent organ damage. Since the discovery of these unusual sickle-shaped red blood cells more than a century ago, our understanding of this illness has advanced tremendously.
Sickle cell anemia is an autosomal recessive genetic disorder, which means that both parents must carry the abnormal gene for a child to inherit the disease. If only one parent carries the gene, the child will be a carrier, but not necessarily affected by the disease. Hemoglobin is a protein in red blood cells responsible for carrying oxygen throughout the body. In individuals with sickle cell anemia, the presence of hemoglobin S causes red blood cells to take on a rigid, crescent or sickle shape when oxygen levels are low, such as during physical exertion or when oxygen demand is high. Over time, the repeated blockage of blood vessels can cause significant organ damage, including to the spleen, liver, lungs, and brain. People with sickle cell anemia are also at increased risk of stroke and various other health problems.
There is a scarcity of epidemiological evidence regarding SCD. It is generally known that sub-Saharan Africa has higher rates of both SCD and HbAS, with HbAS carriers having a natural defense against severe Plasmodium falciparum malaria. Around 230,000 babies with SCA and over 3.5 million newborns with HbAS are thought to have been born in sub-Saharan Africa in 2010. Sub-Saharan Africa is thought to be the birthplace of 75% of babies with sickle cell disease. The majority of people with HbSC illness live in West Africa.
Roughly 100,000 Americans are thought to have sickle cell disease (SCD), according to the US Center for Disease Control (CDC). Additionally, according to the CDC, 1 in 365 African Americans and 1 in 13 newborns born to parents of African American descent have sickle cell disease (SCD). It is estimated that 1 in 16,300 Hispanic Americans have SCD. In the US, up to 40% of SCD patients are children and teenagers. States and the geographic areas where ethnic groups are concentrated affect the incidence. In addition, immigration from abroad and domestic mobility affect the prevalence of SCD and HbAS. This is accurate for patients with SCD and SCA residing in a number of nations.
Hemolysis and vaso-occlusive crisis (VOC) are the two primary characteristics of sickle cell anemia (SCA). Because of a beta-globin gene deficit, sickle hemoglobin (HbS) molecules are more likely to change into stiff, elongated polymers in a deoxygenated environment. At first, sickle erythrocytes go through a cyclical process in which they alternate between the normal biconcave shape and the abnormal crescent shape (which is developed at low oxygen pressure).
Deoxygenation encourages HbS polymerization and is caused by a number of sickle erythrocyte-specific variables, including poor oxygen affinity of HbS, physiologically elevated 2,3-diphosphoglycerate, and elevated sphingokinase-1 activity. The likelihood of HbS polymerization is further increased by excessive HbS concentrations, aberrant Gados channel activity that causes dehydration, and recurrent injury to the membrane of red blood cells (RBCs).
By causing HbS to autooxidize and causing damage to the erythrocyte cell membrane, oxidative stress plays a role in hemolysis. Within sickle RBCs, oxidative stress is elevated due to decreased expression of NADPH oxidase and increased expression of xanthine oxidase and dehydrogenase.
Hemoglobin (Hb) is a significant protein found in red blood cells (RBCs). It consists of four globin chains, with two originating from alpha-globin (located on chromosome 16) and two from beta-globin (located on chromosome 11). There are various subtypes of Hb. The most common ones in adults who do not have hemoglobin disorders are as follows:
The sickle cell mutation arises when a negatively charged amino acid, glutamine, is replaced by a neutral amino acid, valine, at the sixth position of the beta-globin chain. This mutation follows Mendelian genetics and is inherited in an autosomal codominant manner. When someone has two copies of this mutation (homozygous), it results in the most severe form of sickle cell disease, known as SCA or HBSS disease. When beta-thalassemia and the sickle cell mutation are inherited together, it leads to HBS-Beta-0 disease, which has similar characteristics to HBSS disease.
On the other hand, inheriting one copy of the mutation (heterozygous) leads to the HbAS genotype. Individuals with HbAS are typically not considered to have the full spectrum of sickle cell disease, as many of them do not exhibit the usual symptoms of SCA. They may only be identified during events like childbirth, blood donation, or screening procedures.
Prognostic factors in sickle cell anemia (SCA) are elements or characteristics that can be utilized to anticipate how the disease will progress and what the outcome will be for individuals. These factors are valuable in gauging the seriousness of SCA and aiding in making treatment decisions. Key prognostic factors for sickle cell anemia encompass:
Sickle Cell Anemia (SCA) typically involves a combination of clinical assessment, laboratory tests, and genetic testing. However, there are other medical conditions and hemoglobinopathies that can present with similar symptoms or features, making it important to consider a differential diagnosis.
Other Hemoglobinopathies:
Hereditary Spherocytosis:
Hemolytic Anemias:
Iron-Deficiency Anemia:
Thalassemia Minor (Trait):
Other Hemoglobinopathies:
Infections:
Autoimmune Disorders:
Bone Marrow Disorders:
Hypoxia-Induced Symptoms:
The treatment paradigm for sickle cell anemia (SCA) encompasses addressing both immediate and long-term issues. Here is a concise overview of the key elements of this treatment plan:
Education and Genetic Counseling:
Complication Prevention:
Transplantation:
Supportive Care:
Psychosocial Support:
Managing Acute Complications:
Managing Chronic Pain:
Acute Chest Syndrome (ACS):
Sequestration Crises:
Acute Stroke:
Aplastic Crises:
Other Complications:
Chronic Complications:
Iron Overload:
Blood Transfusion:
This comprehensive treatment approach underscores the importance of personalized care and the collaboration of multiple healthcare specialties to ensure the best possible outcomes for individuals living with sickle cell anemia.
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
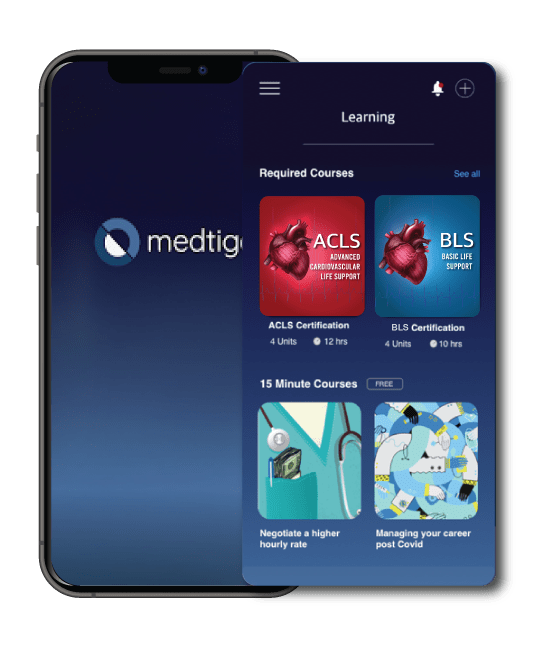
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
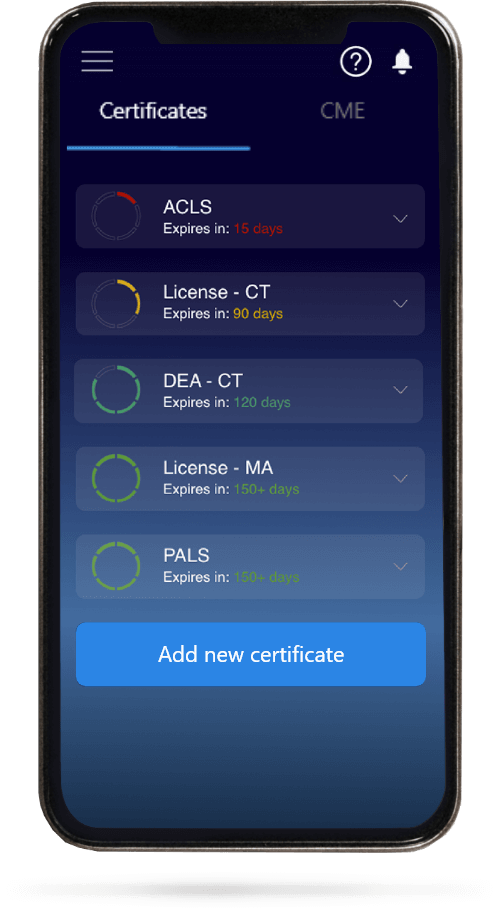
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.