
Monkeypox is a virus from the family Poxviridae that manifests within 5–21 days after exposure. It affects humans and a few animals, and its symptoms include swollen lymph nodes, fever, and a rash with blisters.
In 1958, monkeypox was detected for the first time when monkeys sent to a Danish research facility from Singapore contracted the illness. The first ever human case identified was 12 years later, in 1970. The virus was identified in a child from the Democratic Republic of Congo.
Doctors previously suspected smallpox. Coincidental immunity to this virus was present in individuals who had received the vaccinia vaccine. Still, monkeypox regained clinical relevance due to the eradication of smallpox because vaccination efforts for the same were reduced.

A zoonotic disease previously endemic to Western and Central Africa, monkeypox has been found in multiple animals (especially rodents) and humans. Infections have been identified in prairie dogs, humans, mice, rats, and squirrels.
Until recently, most cases of monkeypox have been isolated to Western Africa, except for a few clusters found in the UK and the midwestern US.
Now several cases can be seen in non-endemic countries, due to which this disease has become a major cause of concern. The disease is self-limiting, and death occurs in severe cases only. The reported case fatality rate is 3–6%.

Transmission of monkeypox can happen through contact with respiratory droplets, skin lesions, or bodily fluids of infected animals or humans.
The disease can also spread from an infected mother to the womb through the placenta.
Individuals who are in close contact with infected patients are at a greater risk for infection, and the chain of successive person-to-person infections has just been increasing over the years. Terminating the smallpox vaccine is probably the main factor behind this.

The first five days of the illness, called the program stage, have the following symptoms:
The characteristic rash of monkeypox develops 1-3 days from the onset of fever, lasting from 2 weeks to 1 month.
The lesions are well circumscribed and deep-seated with a navel-like depression. They’re painful until they begin healing in the crust stage.
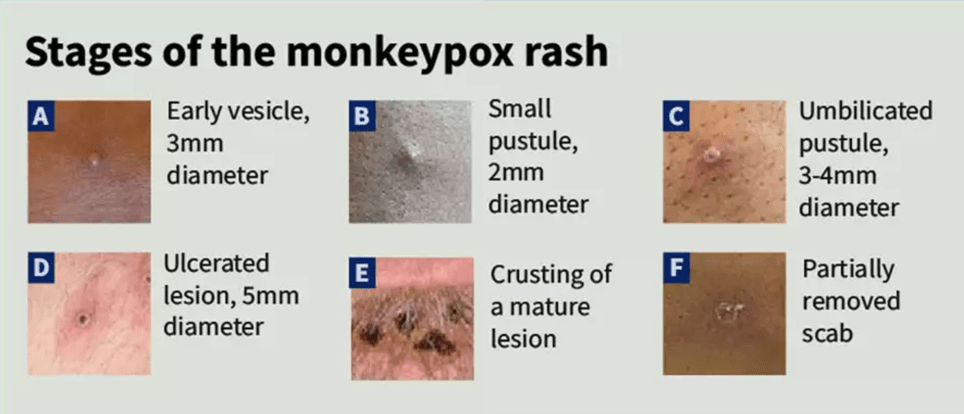
Given below are the stages of the rash:
After healing, there are hypo and hyperpigmented atrophic scars, hypertrophic scarring of the skin, and the contracture of facial muscles following the healing process of ulcerated lesions of the face.

If the individual has been exposed to the virus but remains asymptomatic, they need to be observed for 21 days.
If any symptoms develop, specimens should be collected as per the duration of the illness. Specimens must be collected from multiple locations.
The following specimens must be obtained from symptomatic patients:
The standard laboratory test for monkeypox is PCR detection of virus DNA.
The ideal diagnostic specimens would be those obtained from the rash—skin, crusts, or fluid—and biopsy if available.
Antibody and antigen test methods may be ineffective since they cannot differentiate amongst orthopoxviruses.

There are currently no clinically proven treatments for this infection. As with most viral infections, treatment consists of symptom management. However, there are preventative steps that can aid in preventing an outbreak.
The infected person should wear a triple-layered mask, cover all lesions, and remain isolated until all crusts have gone off spontaneously and a layer of skin has grown. Due to the recognized top limit of the monkeypox incubation period, exposed individuals should check their symptoms and temperature twice a day for 21 days.
Infection coincides with the development of symptoms; consequently, close contacts do not require isolation if asymptomatic but should refrain from donating cells, tissues, organs, or semen for 3 weeks.

In some instances, post-exposure immunization with modified vaccinia, such as the Ankara vaccine, is recommended.
Close skin in contact with an infected patient’s bodily fluids, scabs, or respiratory droplets constitutes a high exposure risk, necessitating immediate post-exposure immunization.
According to the CDC, vaccination may prevent disease onset if administered four days after exposure, and if administered within 14 days, disease severity may be reduced.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.






