Sleepless and Costly: How OSA Is Hitting US and UK Workforces
March 3, 2026
Background
Skin and skin structure infections (SSSIs) make up to about 10% of hospital visits in the U.S. These include deeper infections like necrotizing fasciitis, myositis, and gas gangrene and milder infections like erysipelas, cellulitis, boils, small abscesses, and wound infections. Treatment depends on the cause of infection or injury. The choice of antibiotic depends on the severity of infection. Unfortunately, few antibiotics effectively treat resistant bacteria in serious skin infections. However, novel treatment regimens are being researched to improve available treatments.
Epidemiology
Skin and soft tissue infections affect many people in the U.S. Fourteen million people suffer every year due to these skin infections. Males, black individuals, and those aged 18 to 44 are affected most. Community acquired MRSA leads to 59% of emergency treatments.
Anatomy
Pathophysiology
Microbial pathogens: Many microbes like bacteria, fungi, viruses, and parasites cause SSSIs. The most common are bacteria like Streptococcus pyogenes and Staphylococcus aureus. These include drug resistant strains like MRSA. Sometimes other bacteria are also involved, like Pseudomonas aeruginosa, Enterococcus species, and anaerobic bacteria. Fungi like Candida, Trichophyton, Epidermophyton, and Microsporum can infect skin. Common viruses are HPV, chickenpox, and herpes simplex viruses. Head lice and scabies mites are parasitic pests.
Disruption of skin barrier: SSTIs often arise due to weaker immune systems. This allows germs to enter and grow in the tissue. Trauma, cuts, scrapes, surgery wounds, burns, insect bites, and diseases like psoriasis or eczema can damage the skin barrier. Skin moisture, maceration, and occlusion can also help germs grow and invade.
Inflammatory response: The body reacts to invading germs by starting an inflammatory process. Many immune cells move to the infection site to fight the germs. These cells are neutrophils, macrophages, and lymphocytes. Prostaglandins, cytokines, and chemokines are examples of signaling chemicals. They coordinate the immune response and cause inflammation symptoms such as redness, swelling, heat, and pain.
Production of toxins: Some bacteria produce toxins and other harmful chemicals. They can worsen the skin and tissue infections. For example, S. aureus bacteria can release poisons like PVL (pantone-valentine leukocidin) and hemolysin (alpha-toxin). These break down cells and tissues. They cause abscesses and severe infections that destroy tissue.
Etiology
Many germs cause skin and soft tissue infections. Bacteria like Staphylococcus aureus, Streptococcus pyogenes, Streptococcus agalactiae, Enterococcus species, Pseudomonas aeruginosa, Escherichia coli, Proteus species, and anaerobic bacteria are the main organisms responsible for the infection. Candida species cause a fungal infection called cutaneous candidiasis. Dermatophytoses or tinea infections come from other fungi. Herpes Simplex Virus (HSV), Variola-Zoster Virus (VZV), and Human Papillomavirus (HPV) are viral infections. The mite Sarcoptes scabiei causes scabies. Lice like Pediculus humanus capitis and corporis infect too. These germs lead to skin lesions, secondary bacterial infections, bacterial infections. Identifying and treating these infections can prevent them.
Genetics
Prognostic Factors
Infections of skin and soft tissue may be harmful and severe. The prognosis of the infections depends on various prognostic factors. Skin and soft tissue infections can be serious. Their prognosis depends on several factors. Severity of the disease depends on underlying medical issues, timely treatment, and response to the treatment.
Clinical History
Most SSTI patients have redness, warmth, swelling, and pain. They often have fever and other symptoms also. The legs are most affected areas. Hard lumps form in cellulitis and erysipelas, which spread under the skin. In necrotizing fasciitis, pain exceeds visible issues. Bleeding, fluid-filled sacs, numb areas, rapid spread, and crackling sounds of gas happen. Big swelling and sacs help identify it from milder infections.
Physical Examination
Finding signs of infection on the skin such as redness, swelling, warmth, tenderness, firmness, fluid-filled areas, open sores, and dead tissue. Identify for superficial infections.
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Acute presentation:
Sudden Onset Syndrome is a condition that often comes with sharp pain, swelling, and heat around the injured area. It can also bring fever chills, a general sick feeling, swollen lymph nodes, and inflammation throughout the body. These systemic symptoms are common signs of Sudden Onset Syndrome. The injury site experiences acute discomfort, puffiness, and warm
Subacute presentation:
Infections that are chronic tend to start slowly, over a course of days or even weeks. The symptoms may shift during this period too. Those affected can feel a constant discomfort, of moderate intensity.
Chronic presentation:
Along with persistent symptoms which often intensify despite treatments, chronic surgical site infections may lead to ulcers. They cause granulation tissue growth, delayed wound healing, and secondary infections producing foul-smelling discharge.
Complicated presentation:
Severe pain and tissue necrosis can result from deep surgical site infections. These affect muscles, bones, or fascia. Pus collections, called abscesses, often develop. They need drainage to resolve the problem.
Differential Diagnoses
Inflammatory conditions- contact dermatitis, eczema
Vascular disorders- venous statis dermatitis, arterial insufficiency
Allergic reactions- urticaria, drug eruptions
Dermatological infections- fungal infections, viral infections
Neoplastic conditions- basal cell carcinoma, cutaneous lymphoma
Autoimmune disorders- cutaneous lupus erythematosus, dermatomyositis
Other conditions- deep tissue injuries, arthropod stings, or bites
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
Assessment of symptoms and likely cause of infection leads to proper use of antibiotics. It depends on local resistance patterns, patient factors, and possible germs. For simple skin infections, cephalexin, dicloxacillin, clindamycin, or trimethoprim-sulfamethoxazole pills may be employed. If it is severe or MRSA is suspected, oral or IV drugs could be used. Antibiotics may change based on cultures or worsening symptoms. Proper wound care helps healing and prevents issues. Topical antiseptics or antibiotic ointments treat minor skin infections along with oral antibiotics. Other therapies manage pain, provide support, and address underlying conditions. Patients need close check-ups, follow-ups, and specialist referrals as needed. Prevention means good hygiene, vaccinating against germs, and not sharing personal items.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
Administration of non-pharmaceutical methods to treat skin and skin structure infections
Use of linezolid
Linezolid is a member of novel oxazolidinone derivatives with wide spectrum of activity against gram+ve bacteria including VRE and MRSA. It possesses bacteriostatic action by inhibiting the protein synthesis iin bacteria.
Use of Daptomycin
Daptomycin belongs to cyclic lipopeptide having antimicrbail activity against gram+ve bacteria, enterococci, and staphylococci. It acts by binding to the bacterial membrane via calcium-dependent manner leading to disruption of RNA, DNA and protein synthesis by depolarization leading to the death of bacterial cell.
Use of tigecycline
Tigecycline derived from minocycline is a glycylcycline antibiotic active against gram+ve and gram-ve bacteria.
Use of telavancin
Telavancin, a glycopeptide derived from vancomycin shows bactericidal activity against staphylococci, MRSA and VRSA.
use-of-phases-of-management-in-treating-skin-and-skin-structure-infections
Diagnosing and treating skin infections requires a thorough assessment of the patient’s symptoms, signs, and risk factors. This involves a complete physical exam, medical history review, and diagnostic tests. Treatment includes supportive care, abscess drainage, and empirical antibiotics. Patients need education on preventing recurrence and proper wound care. Monitoring and follow-up are key factors. Optimizing wound healing involves cleaning, debridement, and dressing selection. Preventive measures address risk factors predisposing to infections. For high-risk groups, vaccination against specific pathogens may be considered. Long-term care involves regular surveillance, symptom tracking, and actively managing underlying conditions. Coordinating care with specialists is crucial for minimizing complications and optimizing long-term outcomes.
Medication
Mild/Moderate:
500
mg
twice a day or 250mg 3 times a day
Severe: 875 mg 2 times a day or 500mg 3 times a day
250
mg
Capsule
Orally
every 6 hrs
Complicated: 400mg orally intravenous every day for 7-21 day
Uncomplicated: 400mg orally intravenous every day for seven days
Indicated for Skin structure and complicated skin infections:
4
mg/kg
Lyophilized powder for reconstitution, i
Intravenous (IV)
every 24 hours
7 - 14
days
Dose Adjustments
Renal impairment
Adults with a creatinine clearance (CrCl) of 30 mL/min or greater is 4 mg/kg intravenously (IV) every 24 hours
The recommended dosing for adults with a CrCl less than 30 mL/min is 4 mg/kg IV every 48 hours
For adults undergoing continuous ambulatory peritoneal dialysis (CAPD) or hemodialysis, the recommended dosing is 4 mg/kg IV every 48 hours, administered following hemodialysis on hemodialysis days.
Inidcated for Skin structure and skin infections:
1500mg intravenous once as a single infusion or
1000mg intravenous followed by 500mg intravenous one week later
Infuse intravenously over 30 minutes
Indicated for Skin & Skin Structure Infection:
7.5
mg/kg
Intravenous (IV)
twice a day
7
days
iclaprim (Pending FDA Approval)
Indicated for Acute Bacterial Skin and Skin Structure Infections :
Pending FDA approval
moderate infections:
1-2g intramuscular or intravenous every 8 to 12 hours
severe infections:
2g intravenous every 6 to 8 hours
bacitracin, neomycin, polymyxin B, and hydrocortisone topical
Indicated for Superficial bacterial skin infection:
apply a thin layer of the topical ointment to the affected area 2 to 4 times a day. Use up to 7 days
Indicated for Systemic Fungal Infections:
Test dose: 1 mg Intravenous over 20-30 minutes in 20 mL of 5% dextrose solution
Every 30 minutes for 2 to 4 hours, the patient's temperature, pulse, respiration, and blood pressure must be documented
Loading dose: 0.25mg/kg intravenous everyday
Severe fungal infection: 0.3mg/kg intravenous everyday
Cardio-renal dysfunction or extreme response to test dose: Begin treatment with lower daily dosages, such as 5 - 10 mg
Maintenance: Depending on the patient's cardio-renal state, doses may be progressively raised by 5 to 10 mg daily to 0.5 to 0.7 mg/kg.
Sporotrichosis: Treatment may last up to 9 months, with a total dosage of up to 2.5 g.
Aspergillosis: Therapy may last up to 11 months, with a total dosage of up to 3.6 g.
Dose Adjustments
Renal impairment
CrCl<10ml/min: Administer 0.5-0.7 mg/kg intravenous every 24 to 48 hours
After a dialysis session, provide 0.5-1 mg/kg intravenously every 24 hours for intermittent hemodialysis
Continuous renal replacement therapy: intravenous doses of 0.5–1 mg/kg every 24 hours
Indicated for Skin Structure / Complicated Skin Infections:
500mg intravenous thrice a day
Do not exceed 2g intravenous thrice a day
mix 1-4 drops of lavender oil with a teaspoon of base oil such as almond or olive
it's important to note that the oil mixture should only be used externally or by inhalation
benzalkonium chloride/menthol/petrolatum topical
Scrapes, Cuts, and Burns
First aid for minor wounds, scratches, and burns to prevent skin infection.
Use topically on the affected thrice or four times a day.
Fever Blisters/Cold Sores
Useful in the short-term reduction of discomfort caused by cold sores and fever blisters
Topically apply the affected thrice or four times a day.
Chapped lips
Prevents chapped or cracked lips, provides temporary protection, and aids in their relief.
Topically apply the affected thrice or four times a day.
Dose Adjustments
200 mg orally/intravenously each day for 6 days
Isolates that are susceptible to gram-positive microorganisms
Enterococcus faecalis, Staphylococcus aureus, Streptococcus agalactiae, Streptococcus pyogenes, and Streptococcus anginosus group
Several times a day, the affected area receives a suitable amount of this substance administered to it.
Ophthalmic Drops
Two drops in each eye, three times a day, or half of a single dose.
Use two drops in each eye of the multi-dose eye thrice daily.
Apply thin layer to the affected area once a day
Indicated for Tinea Infection:
Tinea pedis: Apply the cream every night at bedtime or twice a day for 3 to 4 weeks.
Tinea cruris, corporis, and versicolor: Apply the solution or cream every night at bedtime or twice daily for 3 to 4 weeks.
Apply a thin layer into the affected area for 1 to 2 times a day
Indicated for Minor skin irritations
Apply lotion as frequently as necessary to the affected skin area(s)
Apply 1% cream or lotion topically to the affected areas of skin for 2 to 3 times daily
tolnaftate, gentamicin, iodochlorohydroxyquinoline, chlorocresol, betamethasone valerate
Apply topical cream to the affected area twice a day
Apply the required amount on the affected area topically, thrice daily
this medication should not be used on the face for over five days
Topical
Apply the required amount on the affected area topically, thrice daily
this medication should not be used on the face for over five days
Topical
Apply the required amount on the affected area topically, thrice daily
this medication should not be used on the face for over five days
Indicated for Burns, Skin infections, Wounds, Ulcers:
Apply a 0.2% topical treatment to the affected region.
200mg intravenous or oral for one day, followed by 200mg oral per day for one to two weeks.
600 mg Intravenous (IV) twice a day 5 - 14 days
Take 2 to 6 capsules orally daily
Mild/Moderate:
25 mg/kg per day in divided doses every 12hrs or 20 mg/kg per day in equal divided doses every 8hrs
Severe: 45 mg/kg per day divided in doses every 12hrs or 40 mg/kg per day in divided doses every 8hrs
25 - 50
mg/kg
Capsule
Orally
every 8 hrs
10
days
25 - 50
mg/kg
Capsule
Orally
every 8 hrs
10
days
indicated for Skin structure and complicated skin infections:
<1 year: Safety and efficacy not established
1 to <2 years: 10mg/kg intravenous every 24 hours infusion over 30mins
2 to 6 years: 9mg/kg intravenous every 24 hours infusion over 60mins
7 to 11 years: 7mg/kg intravenous every 24 hours infusion over 30mins
12-17 years: 5mg/kg intravenous every 24 hours infusion over 30mins
Indicated for Skin structure and skin infections :
Birth to <6 years: 22.5mg/kg intravenous as a single dose
6 to <18 years: 18mg/kg intravenous as a single dose
Do not exceed 1500mg/dose. Infuse over 30mins
Age: ≥16 years:
7.5
mg/kg
Intravenous (IV)
twice a day
7
days
Indicated for Systemic Fungal Infections:
Test dose: 0.1mg/kg intravenous administered over 20 to 60 minutes. Do not exceed 1mg.
Initial dose: 0.25 mg/kg/dose intravenous every day or every other day
Maintenance: Increase to 1 to 1.5 mg/kg/day in 0.25 mg/day increments as tolerated
Indicated for Skin Structure / Complicated Skin Infections:
≥3 months: 10 mg/kg intravenous thrice a day; Do not exceed 500 mg intravenous every 8 hours
Indicated for fever blisters/cold sores:
≥2 years: Use on the affected region for up to six hours
<2 years: Safety and efficacy not established
For <12 years- Safety and efficacy are not seen
For 12-18 years- 200 mg orally/intravenously each day for 6 days
Isolates that are susceptible to gram-positive microorganisms
Enterococcus faecalis, Staphylococcus aureus, Streptococcus agalactiae, Streptococcus pyogenes, and Streptococcus anginosus group
Indicated for Minor skin infection
Apply lotion as frequently as necessary to the affected skin area(s)
Topical
3 times a day
Apply the required amount on the affected area topically thrice daily
Future Trends
Skin and skin structure infections (SSSIs) make up to about 10% of hospital visits in the U.S. These include deeper infections like necrotizing fasciitis, myositis, and gas gangrene and milder infections like erysipelas, cellulitis, boils, small abscesses, and wound infections. Treatment depends on the cause of infection or injury. The choice of antibiotic depends on the severity of infection. Unfortunately, few antibiotics effectively treat resistant bacteria in serious skin infections. However, novel treatment regimens are being researched to improve available treatments.
Skin and soft tissue infections affect many people in the U.S. Fourteen million people suffer every year due to these skin infections. Males, black individuals, and those aged 18 to 44 are affected most. Community acquired MRSA leads to 59% of emergency treatments.
Microbial pathogens: Many microbes like bacteria, fungi, viruses, and parasites cause SSSIs. The most common are bacteria like Streptococcus pyogenes and Staphylococcus aureus. These include drug resistant strains like MRSA. Sometimes other bacteria are also involved, like Pseudomonas aeruginosa, Enterococcus species, and anaerobic bacteria. Fungi like Candida, Trichophyton, Epidermophyton, and Microsporum can infect skin. Common viruses are HPV, chickenpox, and herpes simplex viruses. Head lice and scabies mites are parasitic pests.
Disruption of skin barrier: SSTIs often arise due to weaker immune systems. This allows germs to enter and grow in the tissue. Trauma, cuts, scrapes, surgery wounds, burns, insect bites, and diseases like psoriasis or eczema can damage the skin barrier. Skin moisture, maceration, and occlusion can also help germs grow and invade.
Inflammatory response: The body reacts to invading germs by starting an inflammatory process. Many immune cells move to the infection site to fight the germs. These cells are neutrophils, macrophages, and lymphocytes. Prostaglandins, cytokines, and chemokines are examples of signaling chemicals. They coordinate the immune response and cause inflammation symptoms such as redness, swelling, heat, and pain.
Production of toxins: Some bacteria produce toxins and other harmful chemicals. They can worsen the skin and tissue infections. For example, S. aureus bacteria can release poisons like PVL (pantone-valentine leukocidin) and hemolysin (alpha-toxin). These break down cells and tissues. They cause abscesses and severe infections that destroy tissue.
Many germs cause skin and soft tissue infections. Bacteria like Staphylococcus aureus, Streptococcus pyogenes, Streptococcus agalactiae, Enterococcus species, Pseudomonas aeruginosa, Escherichia coli, Proteus species, and anaerobic bacteria are the main organisms responsible for the infection. Candida species cause a fungal infection called cutaneous candidiasis. Dermatophytoses or tinea infections come from other fungi. Herpes Simplex Virus (HSV), Variola-Zoster Virus (VZV), and Human Papillomavirus (HPV) are viral infections. The mite Sarcoptes scabiei causes scabies. Lice like Pediculus humanus capitis and corporis infect too. These germs lead to skin lesions, secondary bacterial infections, bacterial infections. Identifying and treating these infections can prevent them.
Infections of skin and soft tissue may be harmful and severe. The prognosis of the infections depends on various prognostic factors. Skin and soft tissue infections can be serious. Their prognosis depends on several factors. Severity of the disease depends on underlying medical issues, timely treatment, and response to the treatment.
Most SSTI patients have redness, warmth, swelling, and pain. They often have fever and other symptoms also. The legs are most affected areas. Hard lumps form in cellulitis and erysipelas, which spread under the skin. In necrotizing fasciitis, pain exceeds visible issues. Bleeding, fluid-filled sacs, numb areas, rapid spread, and crackling sounds of gas happen. Big swelling and sacs help identify it from milder infections.
Finding signs of infection on the skin such as redness, swelling, warmth, tenderness, firmness, fluid-filled areas, open sores, and dead tissue. Identify for superficial infections.
Acute presentation:
Sudden Onset Syndrome is a condition that often comes with sharp pain, swelling, and heat around the injured area. It can also bring fever chills, a general sick feeling, swollen lymph nodes, and inflammation throughout the body. These systemic symptoms are common signs of Sudden Onset Syndrome. The injury site experiences acute discomfort, puffiness, and warm
Subacute presentation:
Infections that are chronic tend to start slowly, over a course of days or even weeks. The symptoms may shift during this period too. Those affected can feel a constant discomfort, of moderate intensity.
Chronic presentation:
Along with persistent symptoms which often intensify despite treatments, chronic surgical site infections may lead to ulcers. They cause granulation tissue growth, delayed wound healing, and secondary infections producing foul-smelling discharge.
Complicated presentation:
Severe pain and tissue necrosis can result from deep surgical site infections. These affect muscles, bones, or fascia. Pus collections, called abscesses, often develop. They need drainage to resolve the problem.
Inflammatory conditions- contact dermatitis, eczema
Vascular disorders- venous statis dermatitis, arterial insufficiency
Allergic reactions- urticaria, drug eruptions
Dermatological infections- fungal infections, viral infections
Neoplastic conditions- basal cell carcinoma, cutaneous lymphoma
Autoimmune disorders- cutaneous lupus erythematosus, dermatomyositis
Other conditions- deep tissue injuries, arthropod stings, or bites
Assessment of symptoms and likely cause of infection leads to proper use of antibiotics. It depends on local resistance patterns, patient factors, and possible germs. For simple skin infections, cephalexin, dicloxacillin, clindamycin, or trimethoprim-sulfamethoxazole pills may be employed. If it is severe or MRSA is suspected, oral or IV drugs could be used. Antibiotics may change based on cultures or worsening symptoms. Proper wound care helps healing and prevents issues. Topical antiseptics or antibiotic ointments treat minor skin infections along with oral antibiotics. Other therapies manage pain, provide support, and address underlying conditions. Patients need close check-ups, follow-ups, and specialist referrals as needed. Prevention means good hygiene, vaccinating against germs, and not sharing personal items.
Dermatology, General
Dermatology, General
Linezolid is a member of novel oxazolidinone derivatives with wide spectrum of activity against gram+ve bacteria including VRE and MRSA. It possesses bacteriostatic action by inhibiting the protein synthesis iin bacteria.
Dermatology, General
Daptomycin belongs to cyclic lipopeptide having antimicrbail activity against gram+ve bacteria, enterococci, and staphylococci. It acts by binding to the bacterial membrane via calcium-dependent manner leading to disruption of RNA, DNA and protein synthesis by depolarization leading to the death of bacterial cell.
Dermatology, General
Tigecycline derived from minocycline is a glycylcycline antibiotic active against gram+ve and gram-ve bacteria.
Dermatology, General
Telavancin, a glycopeptide derived from vancomycin shows bactericidal activity against staphylococci, MRSA and VRSA.
Dermatology, General
Diagnosing and treating skin infections requires a thorough assessment of the patient’s symptoms, signs, and risk factors. This involves a complete physical exam, medical history review, and diagnostic tests. Treatment includes supportive care, abscess drainage, and empirical antibiotics. Patients need education on preventing recurrence and proper wound care. Monitoring and follow-up are key factors. Optimizing wound healing involves cleaning, debridement, and dressing selection. Preventive measures address risk factors predisposing to infections. For high-risk groups, vaccination against specific pathogens may be considered. Long-term care involves regular surveillance, symptom tracking, and actively managing underlying conditions. Coordinating care with specialists is crucial for minimizing complications and optimizing long-term outcomes.
Skin and skin structure infections (SSSIs) make up to about 10% of hospital visits in the U.S. These include deeper infections like necrotizing fasciitis, myositis, and gas gangrene and milder infections like erysipelas, cellulitis, boils, small abscesses, and wound infections. Treatment depends on the cause of infection or injury. The choice of antibiotic depends on the severity of infection. Unfortunately, few antibiotics effectively treat resistant bacteria in serious skin infections. However, novel treatment regimens are being researched to improve available treatments.
Skin and soft tissue infections affect many people in the U.S. Fourteen million people suffer every year due to these skin infections. Males, black individuals, and those aged 18 to 44 are affected most. Community acquired MRSA leads to 59% of emergency treatments.
Microbial pathogens: Many microbes like bacteria, fungi, viruses, and parasites cause SSSIs. The most common are bacteria like Streptococcus pyogenes and Staphylococcus aureus. These include drug resistant strains like MRSA. Sometimes other bacteria are also involved, like Pseudomonas aeruginosa, Enterococcus species, and anaerobic bacteria. Fungi like Candida, Trichophyton, Epidermophyton, and Microsporum can infect skin. Common viruses are HPV, chickenpox, and herpes simplex viruses. Head lice and scabies mites are parasitic pests.
Disruption of skin barrier: SSTIs often arise due to weaker immune systems. This allows germs to enter and grow in the tissue. Trauma, cuts, scrapes, surgery wounds, burns, insect bites, and diseases like psoriasis or eczema can damage the skin barrier. Skin moisture, maceration, and occlusion can also help germs grow and invade.
Inflammatory response: The body reacts to invading germs by starting an inflammatory process. Many immune cells move to the infection site to fight the germs. These cells are neutrophils, macrophages, and lymphocytes. Prostaglandins, cytokines, and chemokines are examples of signaling chemicals. They coordinate the immune response and cause inflammation symptoms such as redness, swelling, heat, and pain.
Production of toxins: Some bacteria produce toxins and other harmful chemicals. They can worsen the skin and tissue infections. For example, S. aureus bacteria can release poisons like PVL (pantone-valentine leukocidin) and hemolysin (alpha-toxin). These break down cells and tissues. They cause abscesses and severe infections that destroy tissue.
Many germs cause skin and soft tissue infections. Bacteria like Staphylococcus aureus, Streptococcus pyogenes, Streptococcus agalactiae, Enterococcus species, Pseudomonas aeruginosa, Escherichia coli, Proteus species, and anaerobic bacteria are the main organisms responsible for the infection. Candida species cause a fungal infection called cutaneous candidiasis. Dermatophytoses or tinea infections come from other fungi. Herpes Simplex Virus (HSV), Variola-Zoster Virus (VZV), and Human Papillomavirus (HPV) are viral infections. The mite Sarcoptes scabiei causes scabies. Lice like Pediculus humanus capitis and corporis infect too. These germs lead to skin lesions, secondary bacterial infections, bacterial infections. Identifying and treating these infections can prevent them.
Infections of skin and soft tissue may be harmful and severe. The prognosis of the infections depends on various prognostic factors. Skin and soft tissue infections can be serious. Their prognosis depends on several factors. Severity of the disease depends on underlying medical issues, timely treatment, and response to the treatment.
Most SSTI patients have redness, warmth, swelling, and pain. They often have fever and other symptoms also. The legs are most affected areas. Hard lumps form in cellulitis and erysipelas, which spread under the skin. In necrotizing fasciitis, pain exceeds visible issues. Bleeding, fluid-filled sacs, numb areas, rapid spread, and crackling sounds of gas happen. Big swelling and sacs help identify it from milder infections.
Finding signs of infection on the skin such as redness, swelling, warmth, tenderness, firmness, fluid-filled areas, open sores, and dead tissue. Identify for superficial infections.
Acute presentation:
Sudden Onset Syndrome is a condition that often comes with sharp pain, swelling, and heat around the injured area. It can also bring fever chills, a general sick feeling, swollen lymph nodes, and inflammation throughout the body. These systemic symptoms are common signs of Sudden Onset Syndrome. The injury site experiences acute discomfort, puffiness, and warm
Subacute presentation:
Infections that are chronic tend to start slowly, over a course of days or even weeks. The symptoms may shift during this period too. Those affected can feel a constant discomfort, of moderate intensity.
Chronic presentation:
Along with persistent symptoms which often intensify despite treatments, chronic surgical site infections may lead to ulcers. They cause granulation tissue growth, delayed wound healing, and secondary infections producing foul-smelling discharge.
Complicated presentation:
Severe pain and tissue necrosis can result from deep surgical site infections. These affect muscles, bones, or fascia. Pus collections, called abscesses, often develop. They need drainage to resolve the problem.
Inflammatory conditions- contact dermatitis, eczema
Vascular disorders- venous statis dermatitis, arterial insufficiency
Allergic reactions- urticaria, drug eruptions
Dermatological infections- fungal infections, viral infections
Neoplastic conditions- basal cell carcinoma, cutaneous lymphoma
Autoimmune disorders- cutaneous lupus erythematosus, dermatomyositis
Other conditions- deep tissue injuries, arthropod stings, or bites
Assessment of symptoms and likely cause of infection leads to proper use of antibiotics. It depends on local resistance patterns, patient factors, and possible germs. For simple skin infections, cephalexin, dicloxacillin, clindamycin, or trimethoprim-sulfamethoxazole pills may be employed. If it is severe or MRSA is suspected, oral or IV drugs could be used. Antibiotics may change based on cultures or worsening symptoms. Proper wound care helps healing and prevents issues. Topical antiseptics or antibiotic ointments treat minor skin infections along with oral antibiotics. Other therapies manage pain, provide support, and address underlying conditions. Patients need close check-ups, follow-ups, and specialist referrals as needed. Prevention means good hygiene, vaccinating against germs, and not sharing personal items.
Dermatology, General
Dermatology, General
Linezolid is a member of novel oxazolidinone derivatives with wide spectrum of activity against gram+ve bacteria including VRE and MRSA. It possesses bacteriostatic action by inhibiting the protein synthesis iin bacteria.
Dermatology, General
Daptomycin belongs to cyclic lipopeptide having antimicrbail activity against gram+ve bacteria, enterococci, and staphylococci. It acts by binding to the bacterial membrane via calcium-dependent manner leading to disruption of RNA, DNA and protein synthesis by depolarization leading to the death of bacterial cell.
Dermatology, General
Tigecycline derived from minocycline is a glycylcycline antibiotic active against gram+ve and gram-ve bacteria.
Dermatology, General
Telavancin, a glycopeptide derived from vancomycin shows bactericidal activity against staphylococci, MRSA and VRSA.
Dermatology, General
Diagnosing and treating skin infections requires a thorough assessment of the patient’s symptoms, signs, and risk factors. This involves a complete physical exam, medical history review, and diagnostic tests. Treatment includes supportive care, abscess drainage, and empirical antibiotics. Patients need education on preventing recurrence and proper wound care. Monitoring and follow-up are key factors. Optimizing wound healing involves cleaning, debridement, and dressing selection. Preventive measures address risk factors predisposing to infections. For high-risk groups, vaccination against specific pathogens may be considered. Long-term care involves regular surveillance, symptom tracking, and actively managing underlying conditions. Coordinating care with specialists is crucial for minimizing complications and optimizing long-term outcomes.
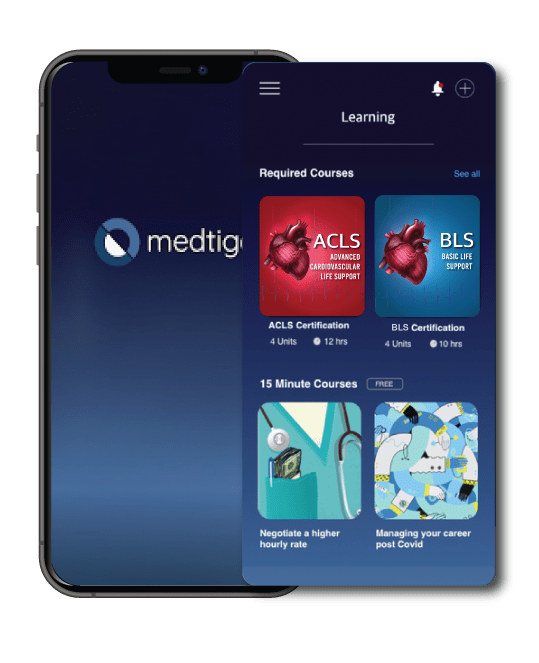
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
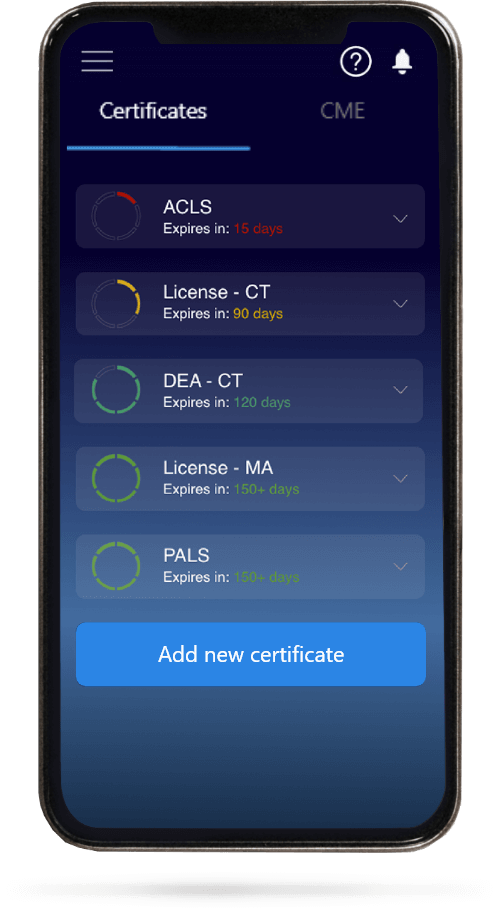
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.