CYP2D6-Guided Opioid Prescribing Fails to Improve Postoperative Pain in ADOPT PGx Randomized Trial
February 23, 2026
Background
Uremia is a condition in which the kidneys are severely damaged and unable to filter waste products and excess fluids from the blood.
Uremia causes fluid, electrolyte, hormone, metabolic abnormalities, and improper kidney function.
It is a common symptom of chronic kidney disease, in its later stages also occur with rapid kidney function loss.
Epidemiology
Uremia prevalence is unknown and hard to determine as patients begin dialysis before experiencing symptoms.
The highest reported prevalence rate for treated ESKD is in Japan, followed by Taiwan and then the United States.
The extent to which a specific racial or ethnic background increases the chances of developing uremia symptoms in patients with equivalent GFRs remains unknown.
Women shows more uremic symptoms at lower creatinine levels due to their lower muscle mass and baseline serum creatinine levels.
Anatomy
Pathophysiology
Anemia-induced fatigue is considered as contributor to the uremic syndrome.
It related with kidney failure causes by a glomerular filtration rate below 50 mL/min.
Bleeding diatheses are common in patients with end-stage kidney disease, which is slightly reduced platelet numbers and increased platelet turnover.
Kidney dysfunctions disrupt the body fluid and electrolyte balance.
Etiology
Certain toxins and environmental pollutants can cause kidney damage and uremia development due to their exposure.
Uremia is caused by chronic kidney disease; it shows gradual decline in kidney function over time.
Study involving 75 patient and 20 healthy individuals of gene expression in ESKD found over 9,000 differentially expressed genes.
Genetics
Prognostic Factors
ESKD patients with uremia have a poor prognosis unless they undergo renal replacement therapy.
CKD shows higher morbidity rates due to comorbid conditions like hypertension and coronary artery disease.
ESKD patients most commonly die from cardiovascular disease, sepsis, cerebrovascular disease.
The risk of complications in the general population is significantly higher in younger patients.
Clinical History
Uremia can affect individuals of all age groups, from infants to elderly individuals.
Physical Examination
Neurological Examination
Cardiovascular Examination
Respiratory Examination
Abdominal Examination
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Uremia spreads rapidly in cases of acute kidney injury due to sudden and severe kidney damage, including dehydration and sepsis.
Uremic symptoms may present only after kidney function suddenly decreases.
Differential Diagnoses
Acute Kidney Injury
Chronic Kidney Disease
Fluid and Electrolyte Imbalances
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
In treatment phase physician should discontinue all medication which causes damage to patient’s renal health.
Renal replacement therapy such as haemodialysis, peritoneal dialysis, and kidney transplant for end-stage renal disease management should implement in patient.
Supportive measures should be considered in cases with severe renal impairment or electrolyte imbalances.
Follow up studies and evaluation of clinical status are required. Appointments with medical physicians and preventing recurrence of infection is an ongoing life-long effort.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
use-of-a-non-pharmacological-approach-for-treating-uremia
Patients should start regular physical exercise to maintain the health.
Patients should increase level of fluid intake during situations where more fluid loss occurs.
Patients should strictly follow a balanced diet including rich in fruits, vegetables, and lean proteins.
Appointments with medical physicians and preventing recurrence of disorder is an ongoing process.
Use of Calcium salts in treatment of uremia
Calcium carbonate: It treats hyperphosphatemia in CKD. They normalize phosphate levels and forms insoluble calcium phosphate excreted in feces.
Calcium chloride: Administer IV injection for cardiac arrhythmias to stabilize myocardial conduction and muscle performance.
Use of Vitamins and Fat-Soluble agents in treatment of uremia
Paricalcitol: It is utilized to treat secondary hyperparathyroidism in ESRD, reduces PTH levels and promotes calcium and phosphorous absorption.
Use of Trace elements in treatment of uremia
Iron dextran: It is utilized to treat microcytic, hypochromic anemia caused by iron deficiency and to replenish iron stores in individuals on erythropoietin therapy.
Ferrous sulfate: It is an essential, inorganic drug that is necessary for hemoglobin formation and the oxidative processes of living tissue.
Use of Phosphate binders in treatment of uremia
Sevelamer: It is a cationic polymer that binds intestinal phosphate, excreted in feces, without absorbing or containing calcium or aluminum ions.
use-of-intervention-with-a-procedure-in-treating-uremia
Hemodialysis involves filtering blood using a dialysis machine to remove waste and excess fluids.
Peritoneal dialysis is a procedure that uses the abdominal peritoneal membrane as a filter to remove waste products and excess fluids from the blood.
Therapies such as continuous renal replacement therapy and kidney transplantation are also used in the treatment of uremia.
use-of-phases-in-managing-uremia
A detailed family history and physical examination of patient is conducted by healthcare specialist in diagnosis phase to identify signs and symptoms of uremia.
Supportive measures including intravenous fluids and electrolyte supplement are given to stabilize and optimize renal function of patient.
The regular follow-up visits with the physician are required to check the improvement of patients and newly observed complaints along with treatment response.
Long-term management phase is a very important phase which involves continuous monitoring, supportive care, and surveillance for late effects of treatment.
Medication
Indicated to treat Atypical Hemolytic Uremic Syndrome to stop complement-mediated TMA (thrombotic microangiopathy)
Loading dose-
For 40-60 kg, 2400 mg intravenously
For 60-100 kg- 2700 mg intravenously
For more than 100 kg- 3000 mg intravenously
Maintenance dose-
Start the maintenance dose 2 weeks later the loading dose
For 40-60 kg, 3000 mg intravenously every 8 weeks
For 60-100 kg- 3300 mg intravenously every 8 weeks
For more than 100 kg- 3600 mg intravenously every 8 weeks
Future Trends
Uremia is a condition in which the kidneys are severely damaged and unable to filter waste products and excess fluids from the blood.
Uremia causes fluid, electrolyte, hormone, metabolic abnormalities, and improper kidney function.
It is a common symptom of chronic kidney disease, in its later stages also occur with rapid kidney function loss.
Uremia prevalence is unknown and hard to determine as patients begin dialysis before experiencing symptoms.
The highest reported prevalence rate for treated ESKD is in Japan, followed by Taiwan and then the United States.
The extent to which a specific racial or ethnic background increases the chances of developing uremia symptoms in patients with equivalent GFRs remains unknown.
Women shows more uremic symptoms at lower creatinine levels due to their lower muscle mass and baseline serum creatinine levels.
Anemia-induced fatigue is considered as contributor to the uremic syndrome.
It related with kidney failure causes by a glomerular filtration rate below 50 mL/min.
Bleeding diatheses are common in patients with end-stage kidney disease, which is slightly reduced platelet numbers and increased platelet turnover.
Kidney dysfunctions disrupt the body fluid and electrolyte balance.
Certain toxins and environmental pollutants can cause kidney damage and uremia development due to their exposure.
Uremia is caused by chronic kidney disease; it shows gradual decline in kidney function over time.
Study involving 75 patient and 20 healthy individuals of gene expression in ESKD found over 9,000 differentially expressed genes.
ESKD patients with uremia have a poor prognosis unless they undergo renal replacement therapy.
CKD shows higher morbidity rates due to comorbid conditions like hypertension and coronary artery disease.
ESKD patients most commonly die from cardiovascular disease, sepsis, cerebrovascular disease.
The risk of complications in the general population is significantly higher in younger patients.
Uremia can affect individuals of all age groups, from infants to elderly individuals.
Neurological Examination
Cardiovascular Examination
Respiratory Examination
Abdominal Examination
Uremia spreads rapidly in cases of acute kidney injury due to sudden and severe kidney damage, including dehydration and sepsis.
Uremic symptoms may present only after kidney function suddenly decreases.
Acute Kidney Injury
Chronic Kidney Disease
Fluid and Electrolyte Imbalances
In treatment phase physician should discontinue all medication which causes damage to patient’s renal health.
Renal replacement therapy such as haemodialysis, peritoneal dialysis, and kidney transplant for end-stage renal disease management should implement in patient.
Supportive measures should be considered in cases with severe renal impairment or electrolyte imbalances.
Follow up studies and evaluation of clinical status are required. Appointments with medical physicians and preventing recurrence of infection is an ongoing life-long effort.
Nephrology
Patients should start regular physical exercise to maintain the health.
Patients should increase level of fluid intake during situations where more fluid loss occurs.
Patients should strictly follow a balanced diet including rich in fruits, vegetables, and lean proteins.
Appointments with medical physicians and preventing recurrence of disorder is an ongoing process.
Nephrology
Calcium carbonate: It treats hyperphosphatemia in CKD. They normalize phosphate levels and forms insoluble calcium phosphate excreted in feces.
Calcium chloride: Administer IV injection for cardiac arrhythmias to stabilize myocardial conduction and muscle performance.
Nephrology
Paricalcitol: It is utilized to treat secondary hyperparathyroidism in ESRD, reduces PTH levels and promotes calcium and phosphorous absorption.
Nephrology
Iron dextran: It is utilized to treat microcytic, hypochromic anemia caused by iron deficiency and to replenish iron stores in individuals on erythropoietin therapy.
Ferrous sulfate: It is an essential, inorganic drug that is necessary for hemoglobin formation and the oxidative processes of living tissue.
Nephrology
Sevelamer: It is a cationic polymer that binds intestinal phosphate, excreted in feces, without absorbing or containing calcium or aluminum ions.
Nephrology
Hemodialysis involves filtering blood using a dialysis machine to remove waste and excess fluids.
Peritoneal dialysis is a procedure that uses the abdominal peritoneal membrane as a filter to remove waste products and excess fluids from the blood.
Therapies such as continuous renal replacement therapy and kidney transplantation are also used in the treatment of uremia.
Nephrology
A detailed family history and physical examination of patient is conducted by healthcare specialist in diagnosis phase to identify signs and symptoms of uremia.
Supportive measures including intravenous fluids and electrolyte supplement are given to stabilize and optimize renal function of patient.
The regular follow-up visits with the physician are required to check the improvement of patients and newly observed complaints along with treatment response.
Long-term management phase is a very important phase which involves continuous monitoring, supportive care, and surveillance for late effects of treatment.
Uremia is a condition in which the kidneys are severely damaged and unable to filter waste products and excess fluids from the blood.
Uremia causes fluid, electrolyte, hormone, metabolic abnormalities, and improper kidney function.
It is a common symptom of chronic kidney disease, in its later stages also occur with rapid kidney function loss.
Uremia prevalence is unknown and hard to determine as patients begin dialysis before experiencing symptoms.
The highest reported prevalence rate for treated ESKD is in Japan, followed by Taiwan and then the United States.
The extent to which a specific racial or ethnic background increases the chances of developing uremia symptoms in patients with equivalent GFRs remains unknown.
Women shows more uremic symptoms at lower creatinine levels due to their lower muscle mass and baseline serum creatinine levels.
Anemia-induced fatigue is considered as contributor to the uremic syndrome.
It related with kidney failure causes by a glomerular filtration rate below 50 mL/min.
Bleeding diatheses are common in patients with end-stage kidney disease, which is slightly reduced platelet numbers and increased platelet turnover.
Kidney dysfunctions disrupt the body fluid and electrolyte balance.
Certain toxins and environmental pollutants can cause kidney damage and uremia development due to their exposure.
Uremia is caused by chronic kidney disease; it shows gradual decline in kidney function over time.
Study involving 75 patient and 20 healthy individuals of gene expression in ESKD found over 9,000 differentially expressed genes.
ESKD patients with uremia have a poor prognosis unless they undergo renal replacement therapy.
CKD shows higher morbidity rates due to comorbid conditions like hypertension and coronary artery disease.
ESKD patients most commonly die from cardiovascular disease, sepsis, cerebrovascular disease.
The risk of complications in the general population is significantly higher in younger patients.
Uremia can affect individuals of all age groups, from infants to elderly individuals.
Neurological Examination
Cardiovascular Examination
Respiratory Examination
Abdominal Examination
Uremia spreads rapidly in cases of acute kidney injury due to sudden and severe kidney damage, including dehydration and sepsis.
Uremic symptoms may present only after kidney function suddenly decreases.
Acute Kidney Injury
Chronic Kidney Disease
Fluid and Electrolyte Imbalances
In treatment phase physician should discontinue all medication which causes damage to patient’s renal health.
Renal replacement therapy such as haemodialysis, peritoneal dialysis, and kidney transplant for end-stage renal disease management should implement in patient.
Supportive measures should be considered in cases with severe renal impairment or electrolyte imbalances.
Follow up studies and evaluation of clinical status are required. Appointments with medical physicians and preventing recurrence of infection is an ongoing life-long effort.
Nephrology
Patients should start regular physical exercise to maintain the health.
Patients should increase level of fluid intake during situations where more fluid loss occurs.
Patients should strictly follow a balanced diet including rich in fruits, vegetables, and lean proteins.
Appointments with medical physicians and preventing recurrence of disorder is an ongoing process.
Nephrology
Calcium carbonate: It treats hyperphosphatemia in CKD. They normalize phosphate levels and forms insoluble calcium phosphate excreted in feces.
Calcium chloride: Administer IV injection for cardiac arrhythmias to stabilize myocardial conduction and muscle performance.
Nephrology
Paricalcitol: It is utilized to treat secondary hyperparathyroidism in ESRD, reduces PTH levels and promotes calcium and phosphorous absorption.
Nephrology
Iron dextran: It is utilized to treat microcytic, hypochromic anemia caused by iron deficiency and to replenish iron stores in individuals on erythropoietin therapy.
Ferrous sulfate: It is an essential, inorganic drug that is necessary for hemoglobin formation and the oxidative processes of living tissue.
Nephrology
Sevelamer: It is a cationic polymer that binds intestinal phosphate, excreted in feces, without absorbing or containing calcium or aluminum ions.
Nephrology
Hemodialysis involves filtering blood using a dialysis machine to remove waste and excess fluids.
Peritoneal dialysis is a procedure that uses the abdominal peritoneal membrane as a filter to remove waste products and excess fluids from the blood.
Therapies such as continuous renal replacement therapy and kidney transplantation are also used in the treatment of uremia.
Nephrology
A detailed family history and physical examination of patient is conducted by healthcare specialist in diagnosis phase to identify signs and symptoms of uremia.
Supportive measures including intravenous fluids and electrolyte supplement are given to stabilize and optimize renal function of patient.
The regular follow-up visits with the physician are required to check the improvement of patients and newly observed complaints along with treatment response.
Long-term management phase is a very important phase which involves continuous monitoring, supportive care, and surveillance for late effects of treatment.
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

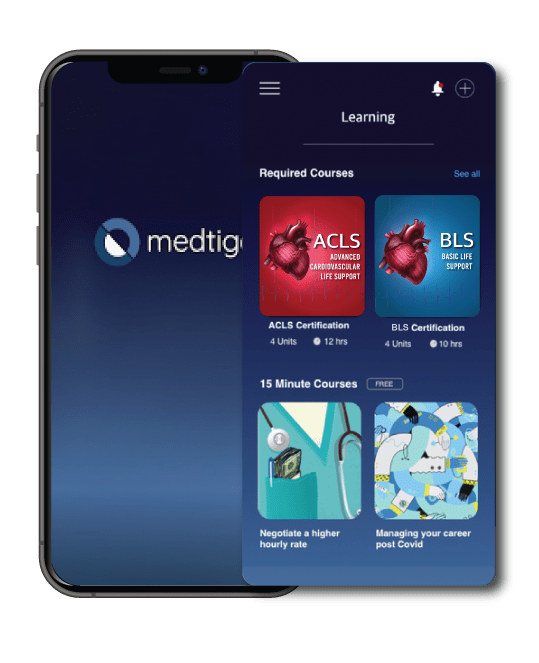
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.




